Objective: Although the experience of pain is multidimentional, and general psychological factors such as anxiety are found to be associated with acute pain, it is necessary to investigate individual emotional variables such as emotional reactivity (ER). The aim of this study was to determine if increased ER is associated with pain during intrauterine device (IUD) insertion even without existing pre-procedure anxiety. Study Design: Prospective cohort study. Methods: We measured the anxiety level in 237 women using the Beck Anxiety Inventory and the ER level using the Emotional Reactivity Scale (ERS) at Zonguldak Maternity Hospital between November 2018 and March 2019. The women rated their pain during IUD insertion. To evaluate the role of ER in the prediction of pain during IUD insertion, we divided the women into subgroups based on the presence of anxiety and level of pain during IUD insertion. Results: ER was higher in women who had anxiety and moderate-severe pain (p = 0.001). In women who were not anxious, ER was higher in those who had moderate-severe anticipated pain or IUD insertion pain than in those who had mild anticipated pain or IUD insertion pain (p = 0.001). In anxious women, the ERS cut-off value was ˃ 34 for predicting the level of pain whereas in non-anxious women, it was ˃ 25. Conclusion: ER is a psychological factor strongly associated with pain at IUD insertion and the ERS appears to be a beneficial tool for detecting ER for this purpose. Health professionals should be aware that psychological factors could contribute to perceived pain more than physiological factors do. Implications: ER is a psychological factor associated with pain at IUD insertion and increased ER is a predictive factor for pain during IUD insertion even without existing pre-procedure anxiety. ERS seems to be a beneficial tool for detecting ER.
The intrauterine device (IUD) can be an ideal, reliable and reversible method for women who require long-term reversible contraception as this approach offers high efficacy (total pregnancy rate of 1.7 per 100 women for the first 3 years of use) [1], low expulsion rate (first-year expulsion rates of the IUD are commonly quoted as 2%-10%) [2], and a lifespan between 5 and 10 years. Despite its well-known efficacy and the fact that it is free of charge in Turkey, it is used by only 17% of women [3]. Several studies have investigated the main barriers to IUD insertion and concluded that fear, pain during insertion and anxiety were the most common obstacles to its use [4, 5]. Nulliparity, not currently breast feeding, older age, history of dysmenorrhea, and lengthier time since last pregnancy are factors reported to be associated with more significant pain [6, 7, 8]. Although the effects of pain during IUD insertion are well established, knowledge is scant about the psychological contributors to the perceived pain during IUD insertion, which can be different from actual pain. A recent study by us demonstrated that experience of cesarean delivery and pre-procedure anxiety were associated with higher pain scores during IUD insertion, and the presence of negative perceptions of IUDs was the most significant predictor of pain during IUD insertion in parous women [9]. Higher pre-procedure anxiety and higher expected pain during IUD insertion were associated with greater pain in other studies [10, 11].
The experience of pain is multidimensional, and it goes beyond nociceptive stimulation [12]. Although general psychological factors such as depression, distress and anxiety were found to be associated with acute pain, the investigation individual emotional variables and cognitions is necessary [13, 14]. Berna et al. demonstrated that negative emotions were correlated with higher perceived pain and negative mood possibly by altering the pain experience via greater activation of neurocircuitry (in the inferior frontal gyrus and amygdala), which is linked to pain-induced changes in emotion regulation mechanisms [15].
Emotional reactivity (ER) is a component of emotion regulation and increased ER likely predisposes individuals to problems with emotion regulation. ER is the tendency to enter an emotional state characterized by the extension of psychological representation of stressful stimuli after their actual termination. Although several studies have focused on the associations between increased ER and anxiety disorders [16-18], there is little available information about the relationship between acute pain and ER.
The aim of the present study was to investigate the relationship between ER, anxiety and pain during IUD insertion to determine if increased ER is a factor associated with pain during IUD insertion even without existing pre-procedure anxiety.
We conducted a prospective cohort study at Zonguldak Maternity Hospital from November 2018 to March 2019. Eligible participants were: aged 18 to 40 years old, desired IUD placement for contraception, had no history of cervical surgery or psychological disease and had not taken any pain or anxiety drugs before the IUD insertion. Women were excluded if IUD insertion was performed for emergency contraception or if they had absolute contraindications to IUD insertion, the presence of cervical stenosis, or dysmenorrhea. A total of 237 women completed the pre-procedure questionnaires to evaluate their demographic characteristics.
We measured the participant’s level of anxiety using the Beck Anxiety Inventory (BAI) which Turkish validation was performed by Ulusoy et al. [19]. Classification of BAI scores are as follows: minimal anxiety 0 to 7, mild anxiety 8 to 15, moderate anxiety 16 to 25, and severe anxiety 30 to 63. According to scores 78 women were anxious, and 159 women were not anxious.
To measure the levels of ER, we used Emotional Reactivity Scale (ERS) which is a 21-item self-report measure [16]. Responders rate the degree to which each item applies to them on a 5-point Likert-type scale. Higher scores indicate higher levels of ER. ERS has been translated and validated for the Turkish population by Secer et al [20]. To determine the construct validity of the scale, Secer et al. performed exploratory factor analysis. Factor loadings of items number 6, 11, 13, and 17 were found to be less than .30, and these factors were excluded from further analysis [20]. The final ERS consisted of 17 items with a Likert scale ranging from 0 to 3 and raw scores ranging from 0 to 51.
No pre-procedure analgesia was used before the intervention. Pre-procedure evaluations and IUD insertions were done separately and blindly. A copper T380A IUD was used in all participants. While viewing a posted visual analogue scale (VAS), the participants rated their pain at the time of uterine sounding by hysterometer which we have demonstrated is the most painful step in IUD insertion [9]. It was demonstrated that a change of 9 to 14 mm on 100 mm VAS represents the minimal clinically important difference in perceived pain that is reproducible among women experiencing both mild and severe forms of pain [21, 22]. We grouped pain scores into categories of mild (0-30 mm) and moderate-severe (31-100 mm). Whereas 120 women reported mild pain, 117 women reported moderate-severe pain.
To evaluate ER for predicting pain during IUD insertion, we classified 39 women who were anxious (BAI score ≥ 1) and reported mild pain (VAS score 0-30 mm) as group 1, 39 women who were anxious (BAI score ≥ 1) and reported moderate-severe pain (VAS score 31-100 mm) as group 2, 81 women who were not anxious (BAI score = 0) and reported mild pain (VAS score 0-30 mm) as group 3, and 78 women who were not anxious (BAI score = 0) and reported moderate-severe pain (VAS score 31-100 mm) as group 4. A flow chart explaining patient selection is shown in Figure 1.
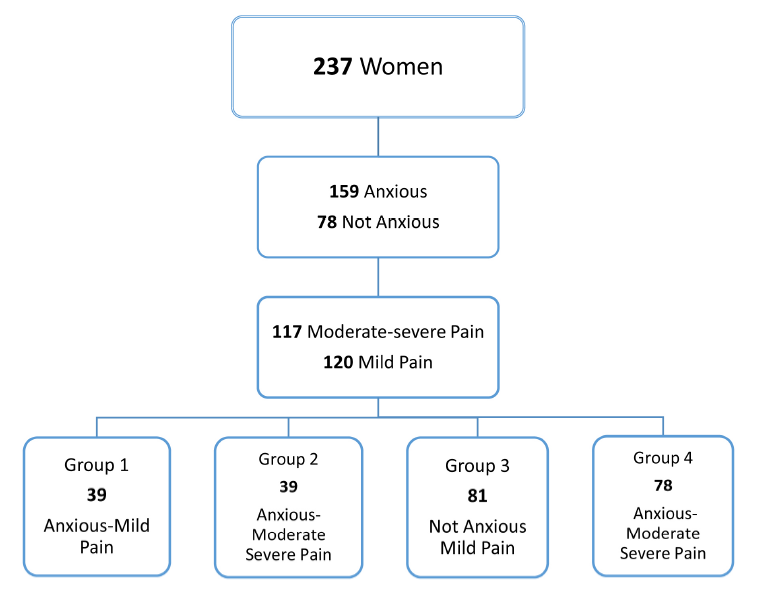 Figure 1.
Figure 1.— Study design flow chart.
IBM SPSS, version 19.0 (IBM, Armonk, NY, US), was used to carry out the statistical analysis. Continuous values were presented with mean, standard deviation (SD), median, minimum and maximum values; categorical variables were presented with frequencies and percentages. The Shapiro-Wilk test was used to test for normality. The independent samples t test or Mann-Whitney U test was used to test whether variables were normally distributed. The Fisher-Yates exact χ2 test was used to compare categorical variables between groups. Multiple linear regression analysis was used to find the best model to predict the stage of highest pain during IUD insertion. All statistical comparisons with a p-value below 0.05 were assumed to be statistically significant. Mann Whitney U and Kruskal Wallis tests used for group comparisons for continuous variables. Youden index calculated with sensitivity and specificity values with 95% CI by ROC analysis for the diagnostic cut-off values of the ERS.
We compared the demographic and clinical characteristics of 120 women who reported mild pain and 117 women who reported moderate-severe pain (Table 1). Although age, body mass index (BMI), occupational status and lactational status were similar among the participants, previous IUD insertion experience was higher in women with mild pain (p = 0.001). Anticipated mean VAS pain scores, mean VAS pain scores at IUD insertion and ER were higher in the patients with moderate-severe pain (p = 0.001). Importantly the BAI scores were similar in the patients who reported mild or moderate-severe pain (4.87 ± 8.02 vs. 4.43 ± 6.60, respectively, p = 0.984).
| Characteristics | Patients with mild pain n (120) |
Patients with moderate-severe pain n (117) |
p valuee |
|---|---|---|---|
| Age* | 33.60 ± 8.40 | 32.77 ± 6.80 | 0.055 |
| BMI* | 29.39 ± 3.84 | 25.57 ± 4.06 | 0.138 |
| Occupation n [%] |
24 [20] | 18 [15.4] | 0.447 |
| Lactating n [%] |
36 [30] | 42 [35.9] | 0.334 |
| Previous IUDa insertion experience | 84 [70] | 42 [35.9] | 0.001 |
| Nulliparity | 27 [22.5] | 39 [33.3] | 0.63 |
| Multiparity | 93 [77.5] | 78 [66.7] | 0.63 |
| Anticipated VASb pain scores* | 23.00 ± 16.68 | 58.71 ± 22.18 | 0.001 |
| VAS pain scores at IUDa insertion* | 15.25 ± 7.09 | 53.00 ± 19.84 | 0.001 |
| ERSc scores* | 17.40 ± 9.44 | 39.84 ± 9.75 | 0.001 |
| BAId scores* | 4.87 ± 8.02 | 4.43 ± 6.60 | 0.984 |
N = no of patients, * Data presented as mean ± SD
a Intrauterine Device, b Visual Analogue Scale, c Emotional Reactivity Scale,d Beck Anxiety Inventory, e Chi-square test.
We regrouped the patients to understand more about the relationship between pain during IUD insertion, ER and anxiety (Figure 1). The demographic characteristics and obstetric history of the women are presented in Table 2. Age, BMI, occupational status and lactational status were similar between the groups. Previous IUD insertion experience was higher in group 3 [anxiety (-), mild pain] women (p = 0.001).
| Characteristics | group 1 anxiety(+) mild pain n(39) |
group 2 anxiety(+) moderate-severe pain n(39) |
group 3 anxiety(-) mild Pain n(81) |
group 4 anxiety(-) moderate-severe pain n(78) |
p value |
|---|---|---|---|---|---|
| Age* | 33.08 ± 5.622 | 32.31 ± 6.005 | 31.99 ± 7.012 | 33.00 ± 7.190 | 0.098 |
| BMI* | 27.46 ± 3.78 | 25.51 ± 3.56 | 25.87 ± 3.78 | 25.61 ± 4.31 | 0.125 |
| Occupation n [%] |
9 [23.1] | 3 [7.7] | 15 [18.5] | 15 [19.2] | 0.306 |
| Lactating n [%] |
9 [23.1] | 15 [38.5] | 27 [33.3] | 27 [34.6] | 0.501 |
| Previous IUDc insertion experience | 18 [46.2] | 15 [38.5] | 66 [81.5] | 27 [34.6] | 0.001 |
| Nulliparity | 9 [23.1] | 15 [38.5] | 18 [22.2] | 24 [30.8] | 0.237 |
| Multiparity | 30 [76.9] | 24 [61.5] | 63 [77.8] | 54 [69.2] | 0.237 |
| Anticipated VASa pain scores* | 26.92 ± 18.80 | 66.92 ± 21.17 | 21.11 ± 15.32 | 54.61 ± 21.66 | 0.001e.g.h.i.j |
| VAS pain scores at IUDb insertion* | 16.92 ± 8.32 | 62.30 ± 24.86 | 14.44 ± 6.32 | 48.07 ± 15.29 | 0.001e.g.h.i.j |
| ERSc scores* | 27.23 ± 7.88 | 44.00 ± 5.04 | 12.66 ± 5.78 | 37.76 ± 10.84 | 0.001e.f.g.h.i.j |
| BAId scores* | 15.00 ± 6.77 | 13.30 ± 3.47 | - | - | 0.496e |
N = no of patients, a Visual Analogue Scale, b Emotional Reactivity Scale, c Intrauterine Device, d Beck Anxiety Inventory.
p values: ebetween groups 1 and 2, fbetween groups 1 and 3, gbetween groups 1 and 4, hbetween groups 2 and 3, ibetween groups 2 and 4, jbetween groups 3 and 4.
*Data presented as Mean VAS score ± SD.
Anticipated mean VAS pain scores were higher in women in group 2 [anxiety(+), moderate-severe pain] than in all other groups (p = 0.001 both; Table 3). In paired comparisons of anticipated mean VAS pain scores between the groups, the only similarity was seen between in group 1 [anxiety(+), mild pain] and group 3 [anxiety(-), mild pain]. Mean VAS pain scores at IUD insertion were also higher in group 2 women [anxiety(+), moderate-severe pain] than all other groups (p = 0.001, both). The same similarity was observed, in anticipated mean VAS scores. In the paired comparisons of mean VAS pain scores at IUD insertion between the groups, the only similarity was seen between women in group 1 [anxiety(+), mild pain] and group 3 [anxiety(-), mild pain]. Importantly, the presence of anxiety did not change the pain outcomes in women who had mild anticipated or mild IUD insertion pain (i.e., groups 1 and 3). Women in group 3 and group 4 had no anxiety and their BAI scores were null. Statistical calculations could not be performed for group 3 or group 4. We observed similar BAI scores in group1 and group 2 (15.00 ± 6.77 vs. 13.30 ± 3.47, p = 0.496).
ER was higher in women in group 2 [anxiety(+), moderate-severe pain] than in all other groups (p = 0,001, both). We established significance in paired comparisons of ER between all groups (p = 0,001 both, Table 2). Among the women who had no pre-procedure anxiety (i.e., group 3 and 4), ER was higher in those who had moderate-severe anticipated or IUD insertion pain (group 4) than in those who had mild anticipated or IUD insertion pain (group 3, p = 0.001).
To determine whether ERS could predict mild or moderate-severe pain, receiver-operating characteristic curve analysis was performed. In anxious women, the ER cut-off value was ˃ 34 with 100% sensitivity (95% confidence interval [CI] 91-100) and 92.31% specificity (95% CI 79.1-98.4). In non-anxious women, the ER cut off value was ˃ 25 with 88.46% sensitivity (95% CI 79.2-94.6) and 100% specificity (95% CI 95.5-100).
We conducted subgroup analysis to further investigate the impact of parity which is a known physiological predictor of pain (Figure 2). In the anxious nulliparous women, the ER cut-off value was ˃ 24 with 100% sensitivity (95% CI 76.8-100) and 66.67% specificity (95% CI 29.9-92.5). In the anxious multiparous women, the ER cut-off value was ˃ 34 with 100% sensitivity (95% CI 85.8-100) and 100% specificity (95% CI 88.4-100). In the non-anxious nulliparous women, the ER cut-off value was ˃ 19 with 88% sensitivity (95% CI 68.8-97.5) and 100% specificity (95% CI 81.5-100). In the non anxious multiparous women, the ER cut-off value was ˃ 25 with 88.9% sensitivity (95% CI 77.4-95.8) and 100% specificity (95% CI 94.3-100).
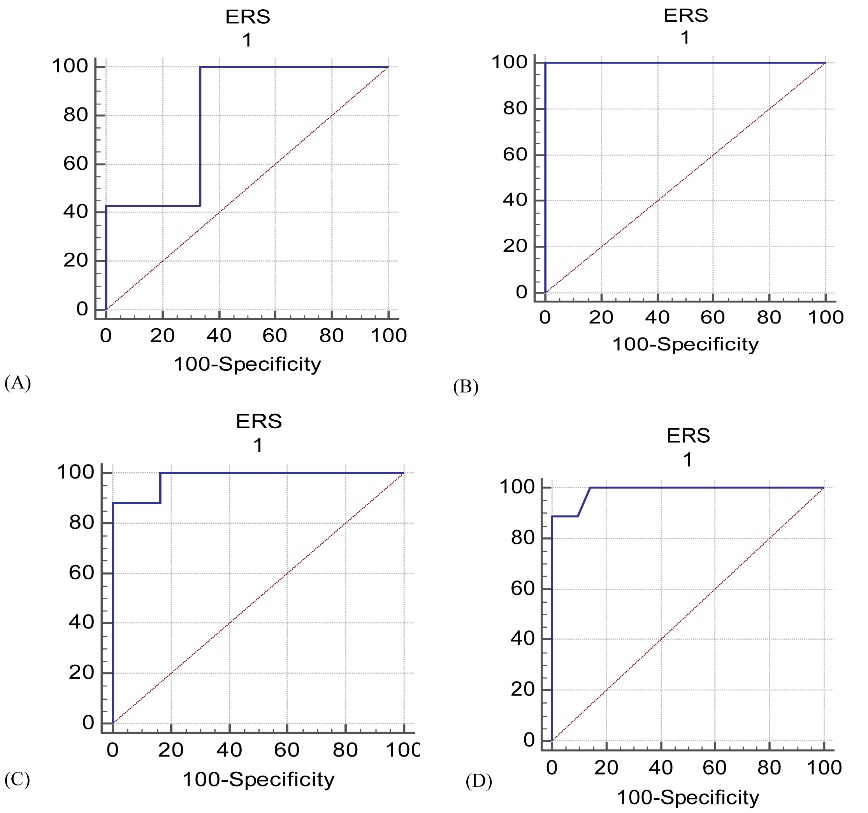 Figure 2.
Figure 2.— ROC Curves of ERS for discrimination of mild or moderate-severe pain. A) Anxious nullipar women, B) Anxious multipar women, C) Non-anxious nullipar women, D) Non anxious multipar women.
We found that the women who had increased ER had more pain at IUD insertion and increased ER was strongly associated with pain in women who were anxious and importantly even non-anxious.
Despite the knowledge of various physiological pain predictors and the fact that local anesthesia was used in most of the previous studies, high pain scores were obtained [23-25]. Shahnazi et al. used aromatherapy to reduce pain at IUD insertion and found no effect. They concluded that pain is a mental feeling and a combination of sensory, emotional, and cognitive components rather than a sign [26].
Another major contributor to pain at IUD insertion was anxiety. It is well known that higher anxiety levels may increase perceived pain to levels worse than the pain actually is [27-29]. A previous study found that women who were more anxious and who anticipated that the procedure would be painful recalled later that it was a painful experience even if they had not experienced any pain during the procedure [4]. The presence of negative perceptions about IUDs, a previous negative history of painful vaginal procedure, or a vaginal examination history that was painful could contribute to pain perception and increase anticipated and actual pain at IUD insertion [9].
Stress and emotional response can affect the pain perception at IUD insertion. Although general psychological factors such as anxiety have been found to modulate pain, some studies investigated pain-specific emotions and cognitions [30, 31]. Ifeagwazi et al. found a relationship between ER and hypertension [32], whereas Marki et al. investigated the relationship between emotion regulation and endometriosis [33]. Our study is the first to demonstrate that increased ER is a factor strongly associated with pain at IUD insertion, even when there was no established anxiety.
The main strengths of our study are that only one physician inserted the same type of IUD to all participants blindly and no pre-procedure medication was used. However, our study was limited by the fact that it did not explore the full variety of psychological mechanisms (e.g., pain hypervigilance, pain anxiety, and pain catastrophizing).
Our study shows that ER, which is a pain specific psychological variable, is strongly associated with pain at IUD insertion. Determining the true predictors of pain is important in patient counselling. Pre-insertion counselling should aim to modulate the woman’s expectation of pain. In addition investigation of the emotional aspect of pain beyond general psychological factors is required to evaluate patients properly and to identify who may benefit from extra reassurance.
In conclusion, ER is psychological factor significantly associated with pain at IUD insertion and ERS appears to be a beneficial tool for the detection of ER for this purpose. Health professionals should be aware that psychological factors can contribute to perceived pain more than physiological factors do. Counseling to inform women of the true benefits and risks of IUDs and providing reassurance to decrease ER and anxiety might be good strategies to manage the pain associated with IUD insertion.
An ethics committee report was obtained from the School of Medicine, Bulent Ecevit University (number: 2018-165-02/10).
The authors declare no competing interests.
