The aims of the study were to investigate the prevalence of anxiety and
depression and to correlate symptoms of anxiety and depression with abnormal
uterine bleeding (AUB) in Korean women. Our study included 124 Korean
premenopausal women aged 15–55 without treatment of psychiatric disorders, who
visited one university hospital due to AUB between September 2015 and December
2019. The Korean Beck Anxiety Inventory (K-BAI) and the Korean Beck Depression-II (K-BDI-II) were used to assess Anxiety and depression symptoms.
We also analyzed obstetrical and clinical data to assess the association between
anxiety and depression with AUB.
The cut-off scores for possible anxiety disorder were met by 37.9% (47 women)
of the patients and for possible depression disorder by 19.5% (24 women). The
most common menstrual associated symptoms were heavy menstrual bleeding (80.6%),
dysmenorrhea (55.6%), and irregular menstrual cycles (33.9%). More women with
AUB in our study had anxiety as measured by the K-BAI and depression as measured
by the K-BDI-II than general Korean population.
A history of abortion and cesarean section (C/sec) were related with anxiety,
whereas a history of minor surgery was related to depression. Anxiety and
depression (r = 0.629, P
Abnormal uterine bleeding (AUB) is defined as an abnormality in the frequency, regularity, amount, or duration of menstrual bleeding and is one of the most common gynecological problems worldwide [1, 2]. Estimates of the prevalence of menstrual problems, such as heavy menstrual bleeding (HMB), intermenstrual bleeding, abnormal menstrual cycles, and premenstrual symptoms, range from 19% to 35% in the general population [3, 4, 5]. Menstrual problems are common among premenopausal women, especially just before and during the perimenopause. AUB can interfere with quality of life and lead women to seek medical care. Although distress and mood disorders have been associated with menstrual problems, the relationship between the two remains unclear. Furthermore, depression and anxiety are probably the two most common psychological symptoms associated with AUB and they can often co-occur leading to a more negative course and outcome [6, 7, 8].
Anxiety and depressive disorders are frequently observed in patients with AUB. Although menstrual problems are not life-threatening, they can impose a significant impact on the quality of life of these patients. Therefore, the identification of these impacts might lead to an understanding of the potential risk of psychological problems and heighten awareness of mental health and associated with women’s health problems [9]. If these negative impacts are identified early, they might lead to prompt recognition and interventions, thus reducing any potential psychological problems.
To the best of our knowledge, no studies have yet examined a potential association between anxiety and depression with AUB in Korean premenopausal women. The purpose of this study was therefore, to identify correlations between anxiety and depression in Korean women with AUB and its goals were to identify (1) general characteristics and menstrual problems, (2) the prevalence and risk of anxiety and/or depression, (3) the correlation between anxiety and depression with AUB (4) and the correlation between AUB with anxiety, and depression according to age.
This study was conducted with 124 consecutive patients who visited the Department of Obstetrics and Gynecology with complaints of menstrual problems and who were diagnosed with AUB between September 2015 and December 2019.
The inclusion criteria were ages between 15 and 55 years (15–20 years, 21–40 years, 41–55 years), and premenopausal women and menstrual irregularities continuing for at least three months. The exclusion criteria included subjects taking psychotropic drugs, such as antidepressants, anxiolytics, or antipsychotics, for any reason in the last six months; a diagnosis of gynecological cancer, currently taking oral contraceptive (OCs), or any hormonal therapy, menopause, and pregnancy. The flow chart in Fig. 1 summarizes the inclusion and exclusion criteria for these patients.
 Fig. 1.
Fig. 1.Flow chart of the participants throughout the trial. AUB, Abnormal uterine bleeding; K-BAI, Korean Beck Anxiety Inventory; K-BDI-II, Korean version of Beck Depression Inventory-II.
The definition of menstrual regularity has changed from one where the shortest
to the longest variation was up to 20 days, to a variation of seven to nine days.
For practical purposes, this normal variation in cycle length can be
alternatively expressed as
After the survey, the patients were followed up for four years and their AUB was treated medically or surgically. Major surgery included total hysterectomy, myomectomy, or ovarian surgery. Minor surgery included endobiopsy, dilatation and curettage, and hysteroscopy.
The self-rated Korean Beck Anxiety Inventory (K-BAI) and the Korean Beck Depression Inventory-II (K-BDI-II) were used to measure self-reported depression and anxiety related symptomatology.
The BAI is a 21-item instrument measuring the severity of anxiety symptoms [13]. The total scores ranged from 0 to 63, with higher scores indicating more severe anxiety symptoms. We used K-BAI and found it showed excellent internal consistency and good discriminant validity for anxiety disorders [6]. The normal range is 0–7 points (minimal), 8–15 points is mild, 16–25 points is moderate, and 26–63 points is severe. The presence of anxiety was determined based on the K-BAI score, and the subjects were classified into normal subjects (K-BAI score range: 0–15) and subjects with anxiety (K-BAI score range: 16–63).
The BDI is a 21-item questionnaire designed to assess the degree of depressive symptoms present over a two-week period. The total score ranges from 0 to 63, with higher scores indicating more severe depressive symptoms. The normal range is 0–3 points, 4–19 points represents mild depression, 20–28 points is moderate, and 29–63 points is severe as defined by the K-BDI-II [14]. The presence of depression was determined based on the K-BDI-II score and the subjects were classified as either normal subjects (BDI score range: 0–19) or depressed subjects (BDI score range: 20–63) in our study.
All statistical analyses were performed using SAS software ver. 9.4 (SAS
Institute Inc., Cary, NC, USA). The Kolmogorov Smirnov test was applied to data
that conformed to a normal distribution. For continuous variables that were not
normally distributed, the significance of the differences between the groups was
tested using the Wilcoxon rank-sum test. The categorical variables were analyzed
using the chi-squared test. Pearson’s correlation and Spearman’s rank correlation
were used to analyze the distribution of the anxiety and depression scores. The
association between anxiety and depression and clinical data were analyzed by
univariable and multivariable logistic regression (anxiety score
From September 1, 2015, to December 30, 2019, a total of 131 women with AUB participated in the survey. Seven patients with psychiatric problems confirmed in the past were excluded, and therefore, the final study was conducted on 124 women with AUB. Informed consent was obtained from the initial 131 women, and the questionnaires were completed, and demographic data and comorbidities were collected from their medical records.
The average age of the cohort was 43.9
Among the patients, 60 women (48.4%) had undergone hysterectomy, five women had undergone myomectomy, 45 women had undergone hysteroscopy or endobiopsy, and 16 women had used the intrauterine device (Mirena). After surgery, the pathological findings revealed that 76 women (61.3%) had uterine disorders (leiomyoma and adenomyosis), 34 women (27.4%) had endometrial disorders (endometrial hyperplasia and endometrial polyps), and three women (2.4%) had endometrial malignancies (atypical endometrial hyperplasia and endometrial cancer).
The most common menstrual problems seen in our study were HMB (n = 100, 80.6%), followed by dysmenorrhea (n = 69, 55.6%) and then irregular menstruation (n = 42, 33.9%, Table 1).
| Total | Anxiety score |
Anxiety score |
P | Depression score |
Depression score |
P | |
| (n = 124) | (n = 77) | (n = 47) | (n = 99) | (n = 24) | |||
| Age (years) | 43.9 |
43.9 |
43.9 |
0.975 | 44.1 |
43.0 |
0.306 |
| BMI (kg/m |
|||||||
| mean |
24.9 |
25.0 |
24.7 |
0.637 | 25.0 |
24.5 |
0.431 |
| 4 (3.2) | 3 (75.0) | 1 (25.0) | 0.678 | 4 (100.0) | 0 (0.0) | 0.499 | |
| 46 (37.1) | 26 (56.5) | 20 (43.5) | 33 (73.3) | 12 (26.7) | |||
| 14 (11.3) | 8 (57.1) | 6 (42.9) | 12 (85.7) | 2 (14.3) | |||
| 60 (48.4) | 40 (66.7) | 20 (33.3) | 50 (83.3) | 10 (16.7) | |||
| Menarche (years) | 14.3 |
14.4 |
14.2 |
0.566 | 14.3 |
14.2 |
0.821 |
| Marriage (%) | |||||||
| no | 23 (18.5) | 15 (65.2) | 8 (34.8) | 0.733 | 18 (78.3) | 5 (21.7) | 0.774 |
| marriage | 101 (81.5) | 62 (61.4) | 39 (38.6) | 81 (81.0) | 19 (19.0) | ||
| Parity (%) | |||||||
| mean |
1.4 |
1.4 |
1.5 |
0.565 | 1.4 |
1.4 |
0.878 |
| 0 | 34 (27.4) | 23 (67.6) | 11 (32.4) | 0.434 | 28 (82.4) | 6 (17.6) | 0.747 |
| 90 (72.6) | 54 (60.0) | 36 (40.0) | 71 (79.8) | 18 (20.2) | |||
| Abortion (%) | |||||||
| mean |
0.9 |
0.8 |
0.9 |
0.094 | 0.8 |
1.2 |
0.163 |
| 0 | 65 (52.4) | 47 (72.3) | 18 (27.7) | 0.014* | 54 (84.4) | 10 (15.6) | 0.257 |
| 59 (47.6) | 30 (50.8) | 29 (49.2) | 45 (76.3) | 14 (23.7) | |||
| Delivery mode (%) | |||||||
| no | 34 (27.4) | 23 (67.6) | 11 (32.4) | 0.132 | 28 (82.4) | 6 (17.6) | 0.373 |
| nsd | 37 (29.8) | 18 (48.6) | 19 (51.4) | 27 (73.0) | 10 (27.0) | ||
| c/sec | 53 (42.7) | 36 (67.9) | 17 (32.1) | 44 (84.6) | 8 (15.4) | ||
| Menstrual regularity (%) | |||||||
| regular | 82 (66.1) | 47 (57.3) | 35 (42.7) | 0.125 | 64 (78.0) | 18 (22.0) | 0.334 |
| irregular | 42 (33.9) | 30 (71.4) | 12 (28.6) | 35 (85.4) | 6 (14.6) | ||
| Dysmenorrhea (%) | |||||||
| no | 55 (44.4) | 33 (60.0) | 22 (40.0) | 0.667 | 44 (81.5) | 10 (18.5) | 0.806 |
| yes | 69 (55.6) | 44 (63.8) | 25 (36.2) | 55 (79.7) | 14 (20.3) | ||
| Heavy menstrual bleeding (%) | |||||||
| no | 24 (19.4) | 15 (62.5) | 9 (37.5) | 0.964 | 19 (79.2) | 5 (20.8) | |
| yes | 100 (80.6) | 62 (62.0) | 38 (38.0) | 80 (80.8) | 19 (19.2) | ||
| History of C/sec (%) | |||||||
| no | 70 (56.5) | 38 (54.3) | 32 (45.7) | 0.041* | 54 (77.1) | 16 (22.9) | 0.282 |
| yes | 54 (43.5) | 39 (72.2) | 15 (27.8) | 45 (84.9) | 8 (15.1) | ||
| History of minor surgery (%) | |||||||
| no | 51 (41.1) | 32 (62.7) | 19 (37.3) | 0.901 | 45 (90.0) | 5 (10.0) | 0.028* |
| yes | 73 (58.9) | 45 (61.6) | 28 (38.4) | 54 (74.0) | 19 (26.0) | ||
| History of OCs (%) | |||||||
| no | 85 (68.5) | 48 (56.5) | 37 (43.5) | 0.057 | 66 (78.6) | 18 (21.4) | 0.431 |
| yes | 39 (31.5) | 29 (74.4) | 10 (25.6) | 33 (84.6) | 6 (15.4) | ||
| History of admission due to AUB (%) | |||||||
| no | 82 (66.1) | 49 (59.8) | 33 (40.2) | 0.453 | 66 (81.5) | 15 (18.5) | 0.699 |
| yes | 42 (33.9) | 28 (66.7) | 14 (33.3) | 33 (78.6) | 9 (21.4) | ||
| History of transfusion (%) | |||||||
| no | 89 (71.8) | 54 (60.7) | 35 (39.3) | 0.603 | 71 (80.7) | 17 (19.3) | 0.931 |
| yes | 35 (28.2) | 23 (65.7) | 12 (34.3) | 28 (80.0) | 7 (20.0) | ||
| History of iron supplementation (%) | |||||||
| no | 45 (36.3) | 27 (60.0) | 18 (40.0) | 0.716 | 34 (75.6) | 11 (24.4) | 0.294 |
| yes | 79 (63.7) | 50 (63.3) | 29 (36.7) | 65 (83.3) | 13 (16.7) | ||
| Hgb (g/dL) | |||||||
| mean |
10.4 |
10.3 |
10.7 |
0.371 | 10.3 |
10.6 |
0.419 |
| Median (range) | 10.5 (4.0–15.9) | 10.2 (4.0–15.6) | 10.8 (4.7–15.9) | 10.2 (5.4–15.9) | 11.2 (4.0–14.5) | ||
| Hct (%) | |||||||
| mean |
32.5 |
32.1 |
33.2 |
0.343 | 32.3 |
33.0 |
0.396 |
| Median (range) | 32.5 (14.9–47.0) | 31.9 (14.9–47.0) | 33.1 (18.7–45.5) | 32.0 (18.8–47.0) | 34.2 (14.9–42.9) | ||
| Medical disorders (DM, HTN, Cancer, thyroid disorder) (%) | |||||||
| no | 93 (75.0) | 56 (60.2) | 37 (39.8) | 0.454 | 75 (80.6) | 18 (19.4) | 0.938 |
| yes | 31 (25.0) | 21 (67.7) | 10 (32.3) | 24 (80.0) | 6 (20.0) | ||
| Data are presented as the n (%) for categorical variable, unless otherwise
indicated. P value for difference were determined by using chi-square or the Wilcoxon rank sum test. *statistically significant as P AUB, Abnormal uterine bleeding; BMI, Body mass index; C/sec, Cesarean section; DM, Diabetes mellitus, HTN, Hypertension. | |||||||
A total of 124 patients underwent the K-BAI assessment and the mean score was
14.2
| Anxiety score | Depression score | ||
| n | 124 | n | 123 |
| Mean |
14.2 |
Mean |
12.7 |
| Median (range) | 12 (0–55) | Median (range) | 11 (0–47) |
| IQR | 6, 19 | IQR | 6, 16 |
| 0–7 | 37 (29.8) | 0–13 | 75 (61.0) |
| 08–15 | 40 (32.3) | 14–19 | 24 (19.5) |
| 16–25 | 27 (21.8) | 20–28 | 16 (13.0) |
| 26–63 | 20 (16.1) | 29–63 | 8 (6.5) |
| IQR, Interquartile Range; K-BAI, Korean Beck Anxiety Inventory; Ocs, Oral contraceptive. | |||
A K-BAI score of 16 or higher was more frequently seen in the AUB group and among women with a history of abortion (P = 0.014, Table 1). Among women who had given birth, 54 (43.5%) had a history of cesarean section (C/sec) and these women reported significantly lower anxiety levels when compared to women with no history of the procedure (P = 0.041, Table 1).
We also analyzed associations between AUB and anxiety according to different age
groups (15–20 years, 21–40 years, 41–55 years, Table S1). In the 21–40 year old
women (n = 24), a higher K-BAI score was associated with the high BMI (23.5
In our study, we performed univariable and multivariable logistic regression of
the K-BAI scores, and clinical and gynecological data (cutoffs: anxiety score
| anxiety score |
depression score | |||||
| Univariable analysis | Multivariable analysis | Univariable analysis | ||||
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | |
| Age (years) | 1.00 (0.95–1.05) | 0.978 | 0.98 (0.93–1.03) | 0.468 | 0.98 (0.93–1.03) | 0.468 |
| BMI (kg/m |
||||||
| 0.55 (0.06–5.08) | 0.601 | 0.30 (0.01–8.34) | 0.476 | 0.30 (0.01–8.34) | 0.476 | |
| reference | reference | reference | ||||
| 0.99 (0.30–3.31) | 0.985 | 0.54 (0.11–2.53) | 0.431 | 0.54 (0.11–2.53) | 0.431 | |
| 1.51 (0.46–4.94) | 0.495 | 0.56 (0.22–1.42) | 0.222 | 0.56 (0.22–1.42) | 0.222 | |
| Menarche (years) | 0.65 (0.30–1.44) | 0.294 | 0.93 (0.66–1.30) | 0.653 | 0.93 (0.66–1.30) | 0.653 |
| Marriage | ||||||
| No | reference | reference | reference | |||
| Yes | 1.15 (0.45–2.96) | 0.768 | 0.80 (0.27–2.40) | 0.697 | 0.80 (0.27–2.40) | 0.697 |
| Parity | ||||||
| 0 | reference | reference | reference | |||
| 1.37 (0.60–3.14) | 0.459 | 1.13 (0.42–3.10) | 0.806 | 1.13 (0.42–3.10) | 0.806 | |
| Abortion | ||||||
| 0 | reference | reference | reference | |||
| 2.48 (1.18–5.23) | 0.017* | 1.65 (0.68–4.04) | 0.270 | 1.65 (0.68–4.04) | 0.270 | |
| Delivery mode | ||||||
| no | reference | reference | reference | |||
| NSD | 2.15 (0.82–5.64) | 0.118 | 1.67 (0.54–5.16) | 0.369 | 1.67 (0.54–5.16) | 0.369 |
| C/sec | 0.98 (0.39–2.45) | 0.965 | 0.84 (0.27–2.61) | 0.760 | 0.84 (0.27–2.61) | 0.760 |
| Menstrual regularity | ||||||
| regular | reference | reference | reference | |||
| irregular | 0.55 (0.25–1.22) | 0.140 | 0.64 (0.24–1.72) | 0.376 | 0.64 (0.24–1.72) | 0.376 |
| Dysmenorrhea | ||||||
| no | reference | reference | reference | |||
| yes | 0.85 (0.41–1.77) | 0.669 | 1.11 (0.45–2.71) | 0.823 | 1.11 (0.45–2.71) | 0.823 |
| Heavy menstrual bleeding | ||||||
| no | reference | reference | reference | |||
| yes | 1.01 (0.40–2.52) | 0.991 | 0.86 (0.29–2.55) | 0.784 | 0.86 (0.29–2.55) | 0.784 |
| History of C/sec | ||||||
| no | reference | reference | reference | |||
| yes | 0.47 (0.22–0.99) | 0.047 |
0.62 (0.25–1.56) | 0.306 | 0.62 (0.25–1.56) | 0.306 |
| History of minor surgery | ||||||
| no | reference | reference | reference | |||
| yes | 1.04 (0.50–2.18) | 0.909 | 2.96 (1.05–8.33) | 0.040* | 2.96 (1.05–8.33) | 0.040 |
| History of Ocs | ||||||
| no | reference | reference | reference | |||
| yes | 0.46 (0.20–1.06) | 0.068 | 0.70 (0.26–1.89) | 0.478 | 0.70 (0.26–1.89) | 0.478 |
| History of admission due to AUB | ||||||
| no | reference | reference | reference | |||
| yes | 0.75 (0.35–1.64) | 0.472 | 1.22 (0.49–3.04) | 0.675 | 1.22 (0.49–3.04) | 0.675 |
| History of transfusion | ||||||
| no | reference | reference | reference | |||
| yes | 0.82 (0.36–1.85) | 0.626 | 1.08 (0.41–2.84) | 0.884 | 1.08 (0.41–2.84) | 0.884 |
| History of iron supplementation | ||||||
| no | reference | reference | reference | |||
| yes | 0.87 (0.41–1.84) | 0.713 | 0.62 (0.25–1.52) | 0.293 | 0.62 (0.25–1.52) | 0.293 |
| Hgb (g/dL) | 1.07 (0.92–1.23) | 0.383 | 1.04 (0.87–1.24) | 0.662 | 1.04 (0.87–1.24) | 0.662 |
| Hct (%) | 1.03 (0.97–1.09) | 0.374 | 1.02 (0.95–1.09) | 0.646 | 1.02 (0.95–1.09) | 0.646 |
| Medical disorders (DM, HTN, Cancer, thyroid disorder) | ||||||
| no | reference | reference | reference | |||
| yes | 0.74 (0.31–1.73) | 0.483 | 1.08 (0.39–2.99) | 0.878 | 1.08 (0.39–2.99) | 0.878 |
| *statistically significant as P AUB, Abnormal uterine bleeding; BMI, Body mass index; C/sec, Cesarean section; DM, Diabetes mellitus; HTN, Hypertension; NSD, Normal spontaneous delivery; Ocs, Oral contraceptive. | ||||||
In the 21–40 year old women, history of minor surgery was associated with
anxiety (OR = 7.04 (1.14–43.36), P = 0.035). In 41–55 year old women,
history of abortion (OR = 2.44 (1.03–5.80), P = 0.043) was associated
with anxiety and high BMI (
There were 73 women (58.9%) with a history of minor surgery and the degree of depression measured by the K-BDI-II was higher than seen in women with AUB who had a history of minor surgery (P = 0.028) in 123 women (Table 1).
In our study, we performed univariable logistic regression of the K-BDI-II
scores, and clinical and gynecological data (cutoffs: depression score
We also analyzed associations between AUB and depression according to different
age groups (15–20 years, 21–40 years, 41–55 years, Table S2). In the 41–55 year
old women (n = 96), a high K-BDI-II score was found in low BMI (25.0
The following factors were not associated with anxiety and depression in 124 women: age, marital status, parity, menstrual regularity, dysmenorrhea, HMB, a history of admission to hospital with AUB, OC use, transfusion history, or iron supplementation, underlying disease, and hemoglobin and hematocrit levels at the time of the assessment.
When the relationship between anxiety and depression was analyzed, Pearson’s
correlation coefficient was found to be r = 0.675 (P
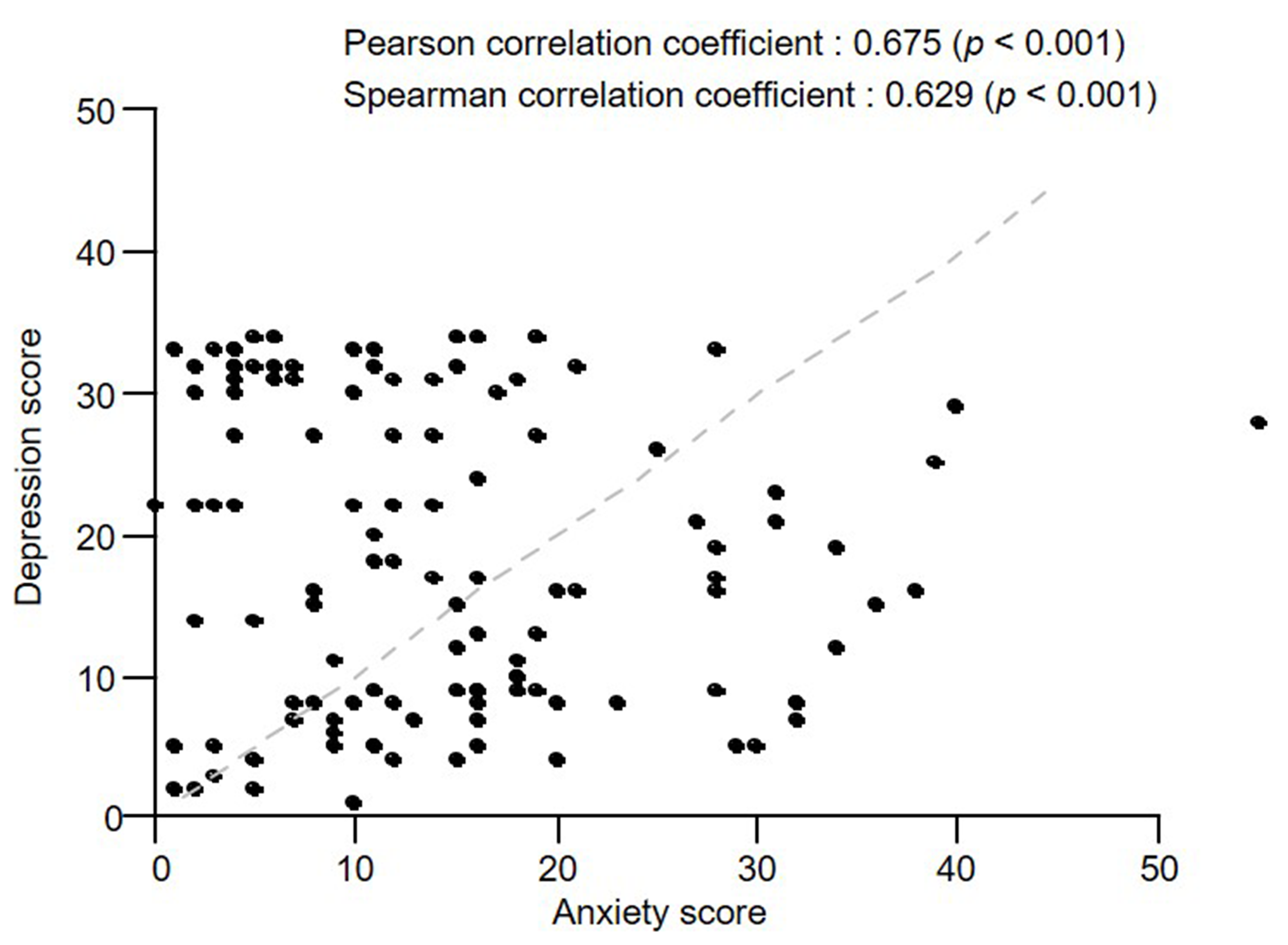 Fig. 2.
Fig. 2.Correlation coefficients for anxiety with depression.
In the present study, two of the most widely used self-reporting assessment instruments for anxiety and depression were used, K-BAI and K-BDI-II, to evaluate the relationships between anxiety, depression and AUB and then used to analyze the association according to age.
The lifetime prevalence of mental illness in the Korean population has been estimated to be 25.4%. According to an epidemiological survey of mental disorders conducted by the Ministry of Health and Welfare, the estimated lifetime prevalence of anxiety disorders for Korean adults was 9.3% (male 6.7%, female 11.7%) and the 1-year prevalence of anxiety disorders in Korean adults was 5.7% (male 3.8%, female 7.5%) [15]. However, the prevalence of major depression is quite wide and ranges between 8.2 and 67%. According to the level of mental health among Koreans, the rate of experience of depression was 13%, and the prevalence of depression was 5.0% [1, 15].
The impact of AUB in reproductive aged women is high, with a prevalence of approximately 3% to 30%. Many published studies have only reported estimates of the prevalence of symptoms of HMB. However, when other symptoms, particularly those associated with irregular and intermenstrual bleeding are included, the prevalence rises to 35% or higher [16].
Several studies have reported that depression is more frequently diagnosed in women during premenstrual, postnatal, and menopausal periods due to fluctuations in hormonal levels [17]. However, it has been difficult to clearly confirm the relationship between psychological aspects and physical symptoms and there are no studies that have looked at the association of AUB with anxiety or depression.
A bidirectional relationship between AUB and psychiatric disorders has been suggested by Kayhan et al. [1]. They reported that psychiatric disorders may play a more important role than AUB. AUB frequently occurs together with stressful events and psychiatric disorders, but once these are resolved, the menstrual cycle becomes regular again. These results are interesting and further research on the relationship between AUB, anxiety and depression are warranted.
The results in this study show a higher percentage of reported anxiety and depression in AUB patients when compared to the general population: 37.9% of the women with AUB reported anxiety measured by the K-BAI, compared to 7.5% in the general population and 19.5% reported depression measured by K-BDI-II compared to 5% in the general population.
Menstrual-related problems (menstrual irregularity, dysmenorrhea, HMB) have been associated with substantial psychological distress. These findings have been confirmed in clinical cases and strongly support the notion that menstrual-related problems may have important public health implications [18, 19]. For example, these problems have been reported by nearly 19% of U.S. women [4]. Furthermore, women with menstrual-related problems have been reported to be 1.7 and 3.0 times more likely to report insomnia, sleepiness, recurrent pain, sadness, nervousness, restlessness, hopelessness, and feelings of worthlessness. Mood and anxiety disorders have frequently been observed in patients with AUB, including major depression (15.6%), generalized anxiety disorder (18.8%), and obsessive-compulsive disorder (22.9%) [1].
Mental illness is highly prevalent among Korean population and AUB plays an important part in aspect of women’s health.
Here, we hypothesized that age, BMI, obesity, abortion history, surgery-related child delivery or gynecological problems, menstruation cycle, dysmenorrhea, anemia, and medical disorders may be associated with anxiety and depression in the presence of AUB.
In our study, history of abortion and C/sec were associated with anxiety disorder (although the interpretation of these findings is difficult, but it seems that anxiety may be connected to the experience of a loss, such as abortion), whereas a history of minor surgery was related to depressive disorder (which seemed to be due to its effect on patient mood in the presence of AUB).
We found that age factor did not affect anxiety and depression associated AUB but there were differences in factors that were influenced by different age groups (15–20 years, 21–40 years, 41–55 years) in anxiety and depression related to AUB.
In anxiety related to AUB, high BMI and history of minor surgery were affected in young women, and BMI, history of abortion, history of C/sec, and Ocs were related in women over 41 years of age.
There was no statistical significance regarding depression, but low BMI and history of minor surgery were associated with women over 40 years of age.
Although our study found no differences in changes in anxiety and depression according to age, it seems necessary to study and analyze the social, physical, and environmental multilateral effects of life as age increases.
Furthermore, anxiety and depression had a moderately positive correlation with AUB, which indicates that it may be wise to closely monitor possible symptom of anxiety and/or depression in women with AUB.
Women with a history of mood disorders were more likely to report heavy bleeding symptoms, independent of known risk factors for heavy bleeding, such as high BMI, fibroids, early perimenopause, and mood disorders. Mood disorder has been shown to be a risk factor for subsequent development of important health disorders, such as diabetes, cardiovascular disease, pain, backache, and dizziness [3, 20]. Mood-related disorders are diverse and affected by several factors.
In AUB patients who visit hospital with anxiety and depression, proper management is necessary, however, the importance of psychological and risk evaluations has been underestimated. Because AUB is affected by age, obstetric history, social environment, and health status, it is difficult to assess their individual contributions to AUB.
There were several limitations to our study. We did not investigate whether psychological distress and adverse health behavior were related to AUB and did not ask for exactly where during the menstrual cycle the psychological and behavioral associations were more profound.
We were unable to determine whether psychological distress and adverse health behaviors were related to AUB and were unable to exactly identify where during the menstrual cycle the psychological and behavioral associations were more profound. The total age range was 15–55 years (although all women were premenopausal), making it difficult to clearly analyze the various effects of age. We were asking for symptoms of possible anxiety and depression in our study using the K-BAI and K-BDI-II. Our study also, could not conclude a causal relationship between menstrual-related problems, emotional well-being, and psychological problems.
The women who participated in the survey are likely to have sampling bias errors because AUB symptoms interfere with daily life. Due to a lack of other similar studies in the literature, an analysis of the difficulties and limitations of the current study in comparison to other studies was not possible.
To the best of our knowledge, this study is the first to examine the correlation between AUB and symptoms of possible mood and anxiety disorders.
Women with AUB seem to be exposed to higher risk of anxiety and depression and furthermore, when there is a history of abortion, C/sec or minor surgery, it is necessary to address the issue of possible anxiety and depression.
Although anxiety and depression were assessed using both K-BAI, K-BDI-II, respectively, this is a meaningful study because it has found that anxiety and depression can be severe in women with AUB. Therefore, including an assessment of AUB as party of the standard evaluation of women, may better enable healthcare providers to recognize and treat potential manifestations of these symptoms.
HNL and MJK designed the research study. HRJ, JMS and GSU performed informed consent from patients. MJK wrote the manuscript. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript.
Ethical approval for the study was obtained from the local ethics committee (HC15QISI0078). The purpose of the study were explained to all participants and written consent was obtained.
Not applicable.
This work was supported by the Institute of Clinical Medicine Research of Bucheon St. Mary’s Hospital, Research Fund, 2020. The statistical consultation (interpretation of data) was supported by a grant (HC14C1062) from the Korea Health Technology R&D Project through the Korean Health Industry Development Institute (KHIDI) funded by the Ministry of Health & Welfare, Republic of Korea.
The authors declare no competing interests.
