Background: Broad ligament leiomyoma is the most common extrauterine leiomyoma, but with a very low incidence rate. When broad ligament leiomyoma is giant and undergoes degeneration, it poses both clinical evaluation and radiological difficulty in differentiating from an ovarian tumor. Meanwhile the changes of anatomical structure increased the difficulty during surgery. Conclusions: Thus, the diagnosis of a cyst-solid complex adnexal mass with a marginally raised serum level of CA125 might be a broad ligament leiomyoma with degeneration besides a ovary tumor. During surgery of myomectomy, we should be meticulous hemostasis and avoid ureter and bladder injury and other complications.
The broad ligament is a double-layered sheet of mesothelial cells originating from 2 layers peritoneal folds and it connects the sides of the uterus to the lateral walls and floors of pelvis. Between the 2 layers tissues, there are connective tissue, smooth muscles, nerves, and blood vessels [1]. Tumors of the broad ligaments are rare. The most common solid tumor of the broad ligament is a leiomyoma [2]. Broad ligament leiomyoma is usually asymptomatic. In uncomplicated cases (e.g., small and no degeneration) broad ligament leiomyoma is clinically interpreted before surgery as a solid adnexal mass which is separated from both the uterine body as well as the ovary. However, if the leiomyoma reaches a significant size, it can lead to various degeneration when the innervation and nutritional status for the leiomyoma changes. Then it may pose greater diagnostic difficulty than when it occurs in the uterus [3]. This is one such case report where a diagnosis of the malignant ovarian tumor was made and finally, the operation and histopathology confirmed the diagnosis of a giant broad ligament leiomyoma with cystic degeneration.
A 46-year-old, married woman, admitted to Qingdao Central Hospital in February 2016 and presented with the complaint of abdominal distension for a month, along with mild abdominal pain. She had no complaints related to menstrual irregularities. The associated complaints of bladder or bowel, anorexia, or weight loss were also not reported. She had one past full-time normal vaginal delivery 22 years ago. Special medical or surgical history and the history for a family member with genital malignancy were not reported. Upon physical examination, her vital signs were normal and we could found an obviously swollen belly as the size of the full-term pregnancy. Abdominal palpation revealed a giant firm mass that extended to the subdiaphragmatic area. No abdominal rebound pain or tenderness was observed. Per vaginal examination revealed a normal vulva, vagina, and vaginal portion of the cervix but fornices were full. Per pelvic examination, we could find a giant cyst-solid mass with a diameter of about 30 cm, the uterus and adnexa were not palpable and we could not determine the mass originated from the uterus or the adnexa.
The laboratory investigation reports showed that hemoglobin was 11.0
g/dL and the serum level of cancer antigen 125 (CA125) was 38 U/mL, while Carcino
Embryonic Antigen (CEA) and serum alpha fetal protein (AFP) and HE 4 levels were
normal. Kidney and liver function tests were within normal limits. Abdominopelvic
computed tomography (CT) scan on 13-02-2016 revealed a well-defined,
heterogeneous, and mixed density mass measuring 35
 Fig. 1.
Fig. 1.(A–B) Abdominopelvic computed tomography scan revealed a well-defined, heterogeneous, and mixed density mass of 35
Exploratory laparotomy was done on 17-02-2016 which revealed a huge
leiomyoma in the right broad ligament. A giant cyst-solid mass was identified
below the abdominal incision intraoperatively (Fig. 2). Firstly, we aspirated
the colorless and transparent fluid contained in the multilocular cystic areas of
the mass surface to reduce the mass volume and enlarge the operative space. Then
the mass which measured about 38 cm
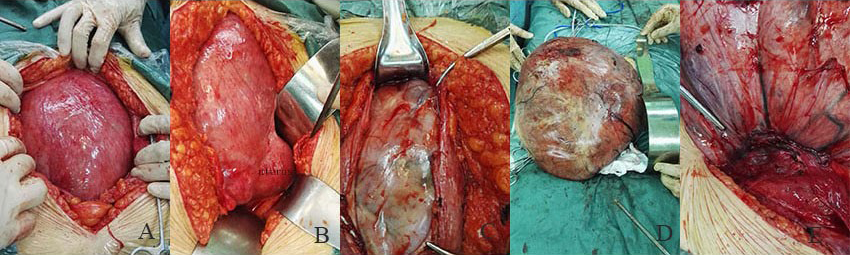 Fig. 2.
Fig. 2.(A–B) Intraoperative findings revealed a normal uterus, bilateral fallopian tubes, bilateral ovaries, and a giant broad ligament leiomyoma. (C–D) The surface of broad ligament leiomyoma showed solid and cystic areas. The solid foci had a brown fleshy homogeneous appearance and the cyst contained colorless and transparent fluid. (E) A large number of prominently dilated nutrient vessels were identified in the root of the broad ligament leiomyoma.
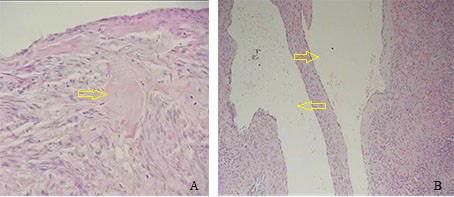 Fig. 3.
Fig. 3.(A) Hematoxylin and eosin stain at
Leiomyoma (also called uterine fibroids) are most often benign, monoclonal,
hormone-dependant tumors composed of uterine smooth muscle interlaced with
connective tissue, and it’s size range from a few millimeters to tens of
centimeters. Approximately 20%–30% of women of reproductive age have
leiomyomas [4], commonly presenting with a variety of symptoms, such as
menorrhagia, pelvic discomfort, urine frequency, dyspareunia or constipation [5].
Broad ligament leiomyoma which is a type of extra-uterine leiomyoma accounts for
6% to 10% of uterine myomas [6] and it can be divided into two types according
to its origin, and one type of leiomyoma which originates from the lateral wall
of the uterine corpus or the cervix and invades the broad ligament is called
false broad ligament fibroid, while the other type which originates from smooth
muscle of round ligament, tubo-ovarian ligament or smooth muscle of uterine
artery or ovarian vessels are called true broad ligament fibroid. Its incidence
is
The giant broad ligament leiomyoma often changed the position of the adjacent organs and vessels during its growth course, and the huge volume of the leiomyoma caused poor exposure during the surgery as well. All those made the surgery more difficult and increase the risk of injury. When working with giant broad ligament leiomyoma, it is necessary to make adequate preparation before surgery, especially to prevent serious bleeding, ureter and bladder injury, and other complications [13]. In the process of surgery, to avoid injury to the right ureter we traced its distribution from the position of the right ureter intersecting with common iliac artery. The right ureter was found in the lower right part of the broad ligament leiomyoma. To avoid injury, we first separated the right ureter from the broad ligament leiomyoma. In our case, we also found a large number of nutrient vessels in the root of the broad ligament leiomyoma, which were easy to cause heavy bleeding during the surgery. Bleeding can easily lead to unclear surgical field and in this condition, the action of clamping blood vessels might increase the probability of ureteral injury. Therefore, in the process of dissecting the broad ligament leiomyoma, the pseudo-capsule close to the tumor body was removed gradually. When happened heavy bleeding, the tumor cavity was quickly packed with large gauze to stop bleeding. The large gauze must be pressed tightly and for enough time. It is forbidden to loosen the pressed gauze frequently to observe whether the bleeding has stopped.
Thus, though uncommon, a giant broad ligament leiomyoma distorting the pelvic anatomy and presenting with atypical ultrasound features should be considered during the evaluation of adnexal masses for optimal patient management. During surgery, we should be meticulous hemostasis and avoid ureter and bladder injury and other complications.
XQW was responsible for the topic of the manuscript, collecting and sorting clinical information, and submission of the manuscript and contact with the editors of the magazine, and most of the writing of the manuscript and subsequent revisions. XFY was responsible for the first draft, TM was responsible for communication and contact with the patient, and LLL was responsible for sorting and confirmation of pathological pictures.
All subjects gave their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of Qingdao central hospital (approval number: [Y]KY202009001).
The authors thank Zhao peng (Biotherapy Center of Qingdao Central Hospital) for the critical reading of this manuscript. I would like to express my gratitude to all those who helped me during the writing of this manuscript. Thanks to all the peer reviewers for their opinions and suggestions.
This research received no external funding.
The authors declare no conflict of interest.
