†These authors contributed equally.
Academic Editor: Graham Pawelec
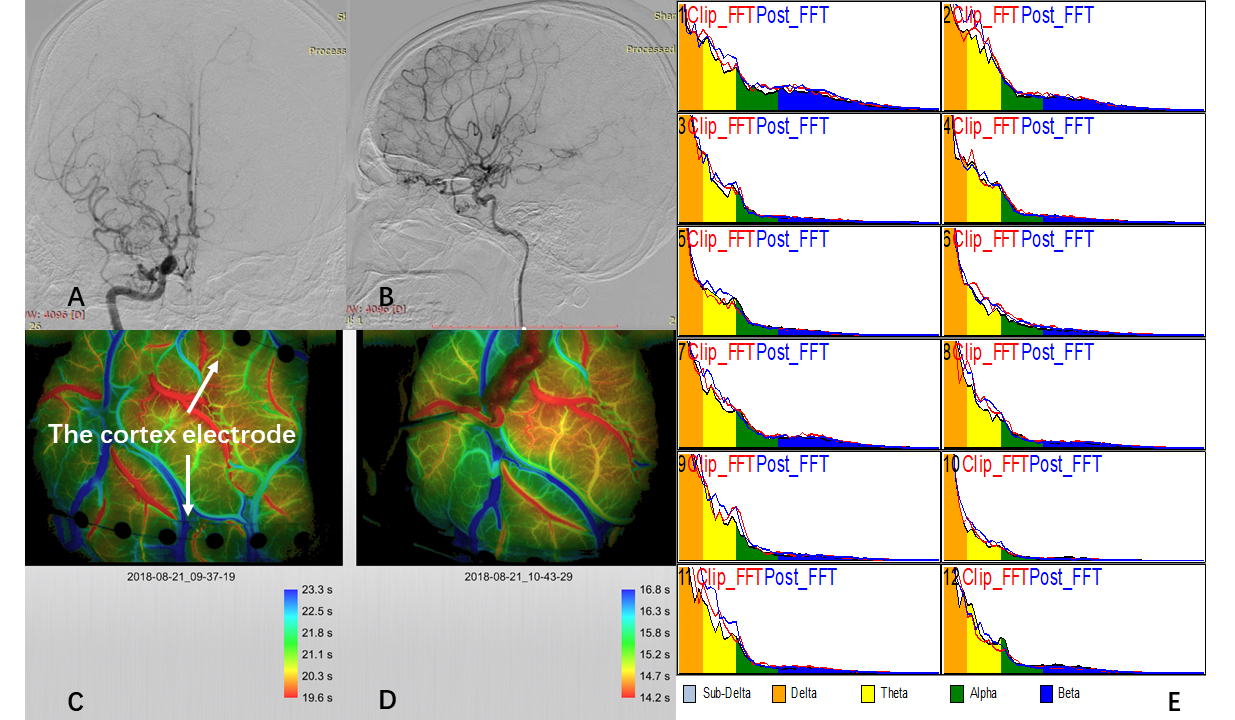
Objective: Postoperative complications of surgical revascularization in
moyamoya disease (MMD) are difficult to predict because of poor knowledge of the
underlying pathophysiological process. Since the aim of surgery is to improve
brain dynamics by increasing regional blood flow, we hypothesize that
postoperative complications are closely related to aberrant electrophysiological
changes. Thus, we evaluated the clinical significance of intraoperative
electrocorticography (iECoG) in bypass surgery for adult MMD. Methods:
Ninety-one adult patients operated on by the same neurosurgeon in our institute
were involved (26 in the iECoG group, 65 in the traditional group). Two 1