Academic Editor: Peter A. McCullough
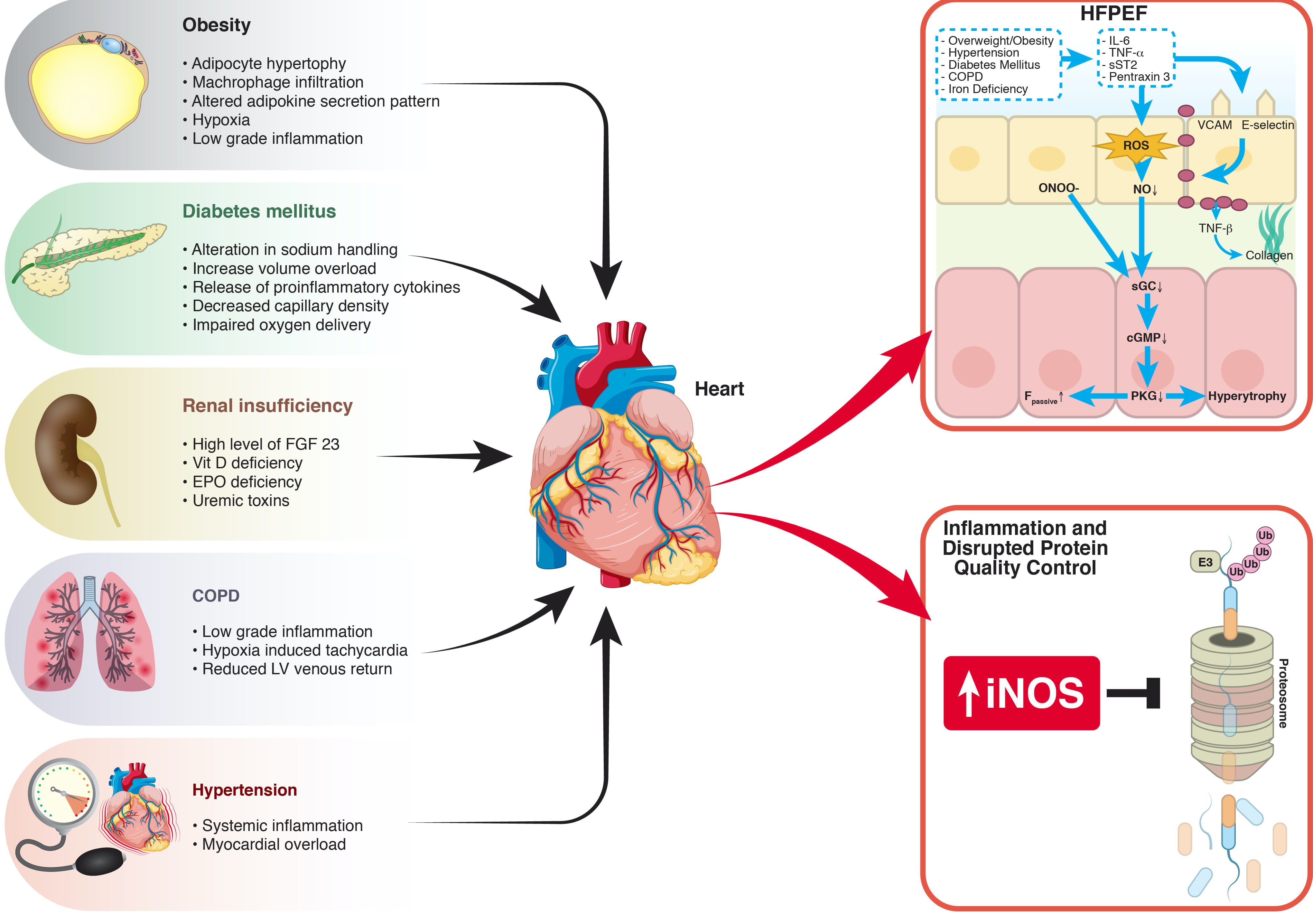
Heart failure with preserved ejection fraction (HFpEF) is one of the greatest unmet needs in modern medicine. The lack of an appropriate therapy may reflect the lack of an accurate comprehension of its pathophysiology. Coronary microvascular rarefaction in HFpEF was first hypothesized in an autopsy study that showed how HFpEF patients had lower microvascular density and more myocardial fibrosis than control subjects. This was later confirmed in vivo when it was noted that HFpEF is associated with reduced myocardial flow reserve (MFR) at single photon emission computed tomography (SPECT) and that coronary microvascular dysfunction may play a role in HFpEF disease processes. HFpEF patients were found to have lower coronary flow reserve (CFR) and a higher index of microvascular resistance (IMR). What is the cause of microvascular dysfunction? In 2013, a new paradigm for the pathogenesis of HFpEF has been proposed. It has been postulated that the presence of a proinflammatory state leads to coronary microvascular endothelial inflammation and reduced nitric oxide bioavailability, which ultimately results in heart failure. Recently, it has also been noted that inflammation is the main driver of HFpEF, but via an increase in inducible nitric oxide synthase (iNOS) resulting in a decrease in unfolded protein response. This review summarizes the current evidence on the etiology of coronary microvascular dysfunction in HFpEF, focusing on the role of inflammation and its possible prevention and therapy.