Academic Editors: Federico Ronco and Jochen Wöhrle
Symptom relief is currently the main indication to perform percutaneous coronary
intervention (PCI) of chronic total occlusion (CTO). So far, none of the
randomized trials for CTO treatment have demonstrated improved survival after
PCI compared to optimal medical treatment (OMT) alone. We investigated whether
CTO PCI in addition to OMT could improve survival over OMT alone. Data of 1004
patients with a treated CTO was analysed. Patients with acute coronary syndrome
and who underwent coronary artery bypass graft surgery (CABG) were excluded, thus
final study population was 378. According to the treatment received, patients
were divided into two groups: CTO PCI + OMT (n = 163) and OMT alone (n = 215).
The primary endpoint was all-cause mortality during follow-up. The incidence of
myocardial infarction (MI), revascularization (both CTO artery and non-CTO artery
related) and stroke were also analysed as a secondary outcome. The mean follow-up
period was 3.55
Chronic total occlusions (CTOs) of coronary arteries are defined as the complete
obstruction of a coronary artery with an occlusion duration of
Data was collected retrospectively from a registry of treated patients in a
single centre (Vilnius University Hospital Santaros klinikos). During the period
of June 2014–December 2018 data of 1004 patients with a treated CTO in one of
the major coronary arteries was analysed. The flow chart of our registry is
demonstrated in Fig. 1. All patients with acute coronary syndromes were excluded
and 470 patients undergoing coronary angiography due chronic coronary syndrome
were further investigated. Patients who underwent CABG (n = 92) were excluded
from further analysis. According to the treatment received, patients were divided
into two groups: those treated by CTO PCI in addition to optimal medical
treatment (n = 163) and those who received optimal medical therapy (OMT) alone (n
= 215). The treatment decision (OMT or PCI + OMT) usually was made together by
the physician and the patient, since there are no hard evidences, which would
favor particular CTO treatment modality. CTO PCI was usually attempted using
antegrade wire escalation technique in most cases; if unsuccessful, the strategy
was changed to antegrade dissection/re-entry or retrograde aproach (mainly
reverse controlled antegrade and retrograde tracking technique). The success rate
of CTO PCI was 89% (successful CTO PCI was performed to 143 of 163 patients).
All patients in both groups received medical treatment as recommended in 2019
European Society of Cardiology (ESC) Guidelines on Chronic Coronary Syndromes
[10]. The primary endpoint investigated was all-cause mortality during follow-up.
The incidence of MI, revascularization (both CTO artery and non-CTO artery
related) and stroke were also analysed as a secondary outcome. The mean follow-up
period was 3.55
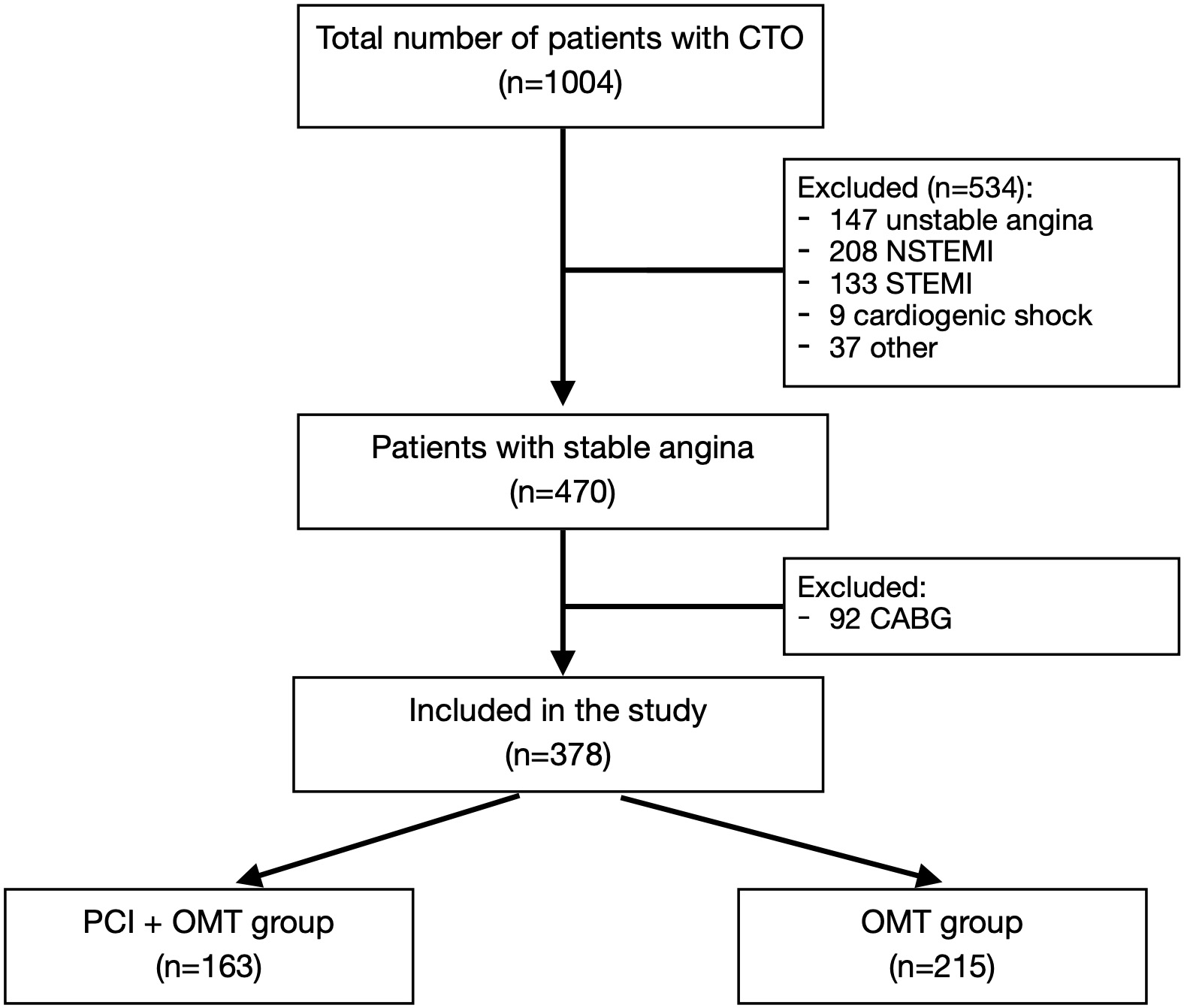 Fig. 1.
Fig. 1.Clinical trial flow chart.
Continuous variables were expressed as mean (
Baseline and demographic characteristics are demonstrated in Table 1. The
majority of patients were male in both groups. Patients treated with PCI were
marginally younger (65.9 years
| Characteristics | PCI, n = 163 | OMT, n = 215 | p |
| Woman sex, no. (%) | 48 (29.4%) | 50 (23.3%) | 0.174 |
| Age, mean |
65.9 |
69.2 |
0.003 |
| Age |
96 (58.9%) | 108 (50.2%) | 0.094 |
| Diabetes mellitus, no. (%) | 51 (31.3%) | 48 (22.3%) | 0.050 |
| Arterial hypertension, no. (%) | 148 (90.8%) | 197 (91.6%) | 0.777 |
| Three-vessel CAD, no. (%) | 43 (26.4%) | 52 (24.2%) | 0.626 |
| Previous MI, no. (%) | 106 (65.0%) | 157 (73.0%) | 0.094 |
| PCI, percutaneous coronary intervention; OMT, optimal medical treatment; SD, standard deviation; MI, myocardial infarction; CAD, coronary artery disease. | |||
Results related to follow-up are presented in Table 2. A mean follow-up period
was 3.55
| Characteristics | PCI, n = 163 | OMT, n = 215 | p |
| Length of follow up, years |
3.56 |
3.55 |
0.845 |
| MI, no. (%) | 11 (6.7%) | 13 (6.0%) | 0.782 |
| CTO vessel MI, no. (%) | 6 (3.7%) | 11 (5.1%) | 0.505 |
| CTO vessel revascularization, no. (%) | 2 (1.2%) | 3 (1.4%) | 0.887 |
| Revascularization, no. (%) | 15 (9.2%) | 15 (7.0%) | 0.428 |
| Stroke, no. (%) | 1 (0.6%) | 2 (0.9%) | 0.731 |
| All-cause mortality, no. (%) | 17 (10.4%) | 41 (19.1%) | 0.021 |
| PCI, percutaneous coronary intervention; OMT, optimal medical treatment; SD, standard deviation; MI, myocardial infarction; CTO, chronic total occlusion. | |||
Prognostic factors of all-cause mortality are presented in Tables 3,4.
Univariate linear regression analysis showed that patients age, presence of
three-vessel CAD and treatment option correlated with all-cause mortality. We
combined these variables in multivariable logistic regression analysis, which
revealed that patients age
| Predictor | p | OR (95% CI) |
| Woman sex | 0.523 | 1.223 (0.659; 2.272) |
| Age | 1.078 (1.042; 1.114) | |
| Age |
0.004 | 0.425 (0.238; 0.758) |
| Diabetes mellitus | 0.363 | 1.328 (0.721; 2.445) |
| Arterial hypertension | 0.331 | 0.644 (0.266; 1.563) |
| Three-vessel CAD | 0.037 | 1.887 (1.040; 3.422) |
| Previous MI | 0.413 | 1.303 (0.692; 2.455) |
| Treatment option (PCI) | 0.023 | 0.494 (0.269; 0.906) |
| CAD, coronary artery disease; PCI, percutaneous coronary intervention; OR, odds ratio; CI, confidence interval. | ||
| Predictor | p | OR (95% CI) |
| Age |
0.011 | 0.466 (0.259; 0.838) |
| Three-vessel CAD | 0.057 | 1.806 (0.982; 3.324) |
| Treatment option (PCI) | 0.032 | 0.508 (0.274; 0.943) |
| CAD, coronary artery disease; PCI, percutaneous coronary intervention; OR, odds ratio; CI, confidence interval. | ||
The present registry was designed in a large interventional cardiology centre with significant PCI and CABG volume. The success rate of CTO PCI was 89%, which is considered high in the contemporary setting. The main finding of our study is that CTO PCI alongside optimal medical treatment is associated with a lower all-cause mortality compared to medical treatment alone. Although OMT patients were marginally older than PCI group patients, multivariate regression analysis has demonstrated that treatment option is an independent predictor of all-cause mortality.
Our registry’s main discovery that CTO PCI is associated with improved survival contrasts to previously performed RCT trials. All the trials we have assessed have some factors, which prevent long term data on survival after CTO PCI being fully evaluated, i.e., the EXPLORE (Evaluating Xience and Left Ventricular Function in Percutaneous Coronary Intervention on Occlusions After ST-Elevation Myocardial Infarction) trial analysed whether patients with ST-Elevation Myocardial Infarction (STEMI) and concurrent CTO in a non-infarct-related artery benefit from additional PCI of CTO shortly after primary PCI [11]. 304 patients were enrolled in this study and the success rate of CTO PCI was 73%. CTO PCI did not result in lower mortality rates compared to medical treatment. However, the EXPLORE trial had a relatively short follow-up of 4 months and we suggest that a longer follow-up is needed in order to investigate any benefit CTO PCI to survival. Similarly, the EuroCTO (A Randomized Multicentre Trial to Evaluate the Utilization of Revascularization or Optimal Medical Therapy for the Treatment of Chronic Total Coronary Occlusions) trial, which enrolled 396 patients, randomly assigned in 2:1 fashion to CTO PCI and OMT alone, did not find a significant difference between groups in respect of all-cause mortality during the 12 month follow up [8]. The largest RCT trial comparing CTO PCI with medical treatment – the DECISION-CTO (Drug-Eluting Stent Implantation Versus Optimal Medical Treatment in Patients With Chronic Total Occlusion) trial has enrolled 834 patients. The median follow-up was 4 years, however, during this relatively long follow-up CTO PCI did not improve survival, as compared to OMT alone [7]. This study however was stopped early due to difficulties with patient enrolment. In addition, the cross-over rate was high (19.6% patients crossed over to receive CTO PCI within 3 days of randomization), and the study was underpowered to detect difference in mortality as an end-point. The IMPACTOR-CTO (Impact on Inducible Myocardial Ischemia of Percutaneous Coronary Intervention versus Optimal Medical Therapy in Patients with Right Coronary Artery Chronic Total Occlusion) trial randomized 94 patients with isolated right coronary artery CTO to PCI or OMT alone [9]. Survival did not differ among the two groups during 12 months follow-up, however, this finding could also be attributed to relatively small patient number and short follow up.
Despite novel tools and techniques used to perform CTO PCI, increasing operator
experience and growing procedural success rate, to date, none of the RCTs
focusing on CTO have ever demonstrated that CTO revasularization improves
survival as compared to medical treatment. The reasons for this may be
multifactorial and include difficulties in achieving significant patient numbers,
relatively high cross-over rates and short follow-up. Selection criteria and
dependent on the chances of a successful PCI may also play a part. Although the
outcomes from RCTs have shown no benefit to survival for CTO PCI a few
observational studies and a meta-analysis have demonstrated that there could be
benefit. Khan et al. [12] performed a meta-analysis of 23 observational
studies comparing patients with successful CTO recanalization and those managed
conservatively. They found that successful recanalization of a CTO results in
improved all-cause mortality (relative risk [RR] of 0.54, 95% confidence
interval [CI] (0.45–0.65), p-value
We conclude that there is a beneficial role for registry data in providing gaps in the knowledge of the clinical relevance of CTO PCI and providing evidence that this form of treatment is effective and can result in longer survival.
The results of our study, however, should be interpreted in a view of certain limitations. First of all, due to limited data in multivariate regression analysis, we cannot ascertain, that all important factors that could contribute to all-cause mortality were identified. We recognise the possibility of selection bias in our study, i.e., the PCI group had a slightly younger average age and possibly their coronary anatomy was more favourable to intervention. Also, we do not have data regarding heart failure status (New York Heart Association (NYHA) class), ejection fraction and myocardial viability. We look forward to the results of larger RCTs such as the ongoing NOBLE-CTO (The NOrdic-Baltic Randomized Registry Study for Evaluation of PCI in Chronic Total Coronary Occlusion) and ISCHEMIA-CTO (Revascularisation or Optimal Medical Therapy of CTO) trials, which should provide some useful insights, however, they are estimated to be completed in 2037 and 2028, respectively.
The data from our centre registry demonstrates that percutaneous coronary intervention of a chronic total occlusion is associated with reduced all-cause mortality as compared to medical treatment alone in a real-life setting.
AB designed the research study. PB wrote original daft. VB, IMS and AB performed the research. VB, IMS and PB analyzed the data. MR, GD, AB and PB reviewed and edited original draft. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript.
The study was conducted in accordance with the Declaration of Helsinki, and the clinical trials committee of our institution approved the protocol (CTO-01/1.1). All patients provided informed consent for treatment according to good clinical practice.
We would like to express our gratitude to all the peer reviewers for their opinions and suggestions.
This research received no external funding.
The authors declare no conflict of interest.
