- Academic Editor
Background: Musculoskeletal pain (MSP) is common among lactating
mothers. The aims of this study were to assess the prevalence of MSP and its
association with the positioning of lactating mothers in Riyadh, Saudi Arabia.
Methods: This was a descriptive cross-sectional survey study using an
online self-administered questionnaire. Results: 336 women aged 20–50
years participated in this study (58.3% reported vaginal delivery, 74.1% had
one to four children, 61.3% had a bachelor’s degree or higher, and 45.5%
worked). Only 25% of the mothers were given health education regarding MSP.
97.3% of mothers reported pain on at least one part of their body. There were
differences in pain intensity ratings across different locations (with a median
and interquartile range in parentheses): lower backs at 0 (0, 6) and upper backs
at 2 (0, 5), necks at 3 (0, 6), shoulders at 3 (0, 5) and arms at 2 (0, 4), and
hands at 1 (0, 4). MSP prevalence ranges from 58.6% for arm and hand to 72.3%
and 67.6% for lower back and neck, respectively. MSP prevalence is significantly
associated with breastfeeding positions (p
Musculoskeletal pain (MSP) refers to pain in the muscles, bones, ligaments, tendons, and nerves [1]. It may present at one site, such as in neck pain, lower back pain, or shoulder pain, or may extend to more than one site [2]. One of the common causes of MSP is postural strain, repetitive movements, overuse, and prolonged immobilization [3].
After giving birth, women often experience musculoskeletal problems due to various factors. These issues can arise as a result of hormonal and physiological changes that occur during pregnancy, as well as postpartum depression and changes in postural habits following childbirth [1, 4, 5]. This is one of the challenges experienced by lactating mothers (i.e., those who breastfeed) as a result of prolonged sitting and non-ergonomic breastfeeding positions [4, 6, 7, 8]. Lactating mothers adopt different positions; some of the common breastfeeding positions are the cradle position (The baby is placed on the mother’s arm on the same side as the nursing breast to hold the baby’s head and body), cross-cradle position (The baby is placed on the mother’s arm opposite the nursing breast to hold the baby’s head and body), side-lying position (Mother and baby lie belly-to-belly on their sides), football hold (also known as the underarm position; The mother sits with the baby resting along the mother’s forearm, with the baby’s body tucked alongside her side, with his feet facing the back of the chair), and laid-back position (The mother reclines with the baby’s body across her chest) [8, 9, 10, 11].
The prevalence of MSP among lactating mothers has been noted to be high in different populations. In Karnataka, India, 99% of postpartum women complained of MSP, with lower back pain being the most common (74%) [6]. Jothi Prasanna and Tamizhmani [7] reported that neck pain was the most common among lactating mothers in Kattankulathu, India, with a prevalence of 61%, followed by (in descending order) pain in the shoulders (59%), upper back (58%), lower back (46%), elbow (41%), and wrist and hand (22%); there was no pain reported in the lower extremities. In another study, among Nigerian lactating mothers, 51.7% reported pain in the neck. In Pakistan, the prevalence of neck pain was 37.3%, and lower back pain was 21.8%; the pain reported in other sites (shoulder, arm, hands, upper back, and legs) did not exceed 6% [8]. In Malaysia, pain in the lower back was reported to be 69.4%, and 58% reported neck pain [11].
Different sociodemographic and maternal characteristic factors have been associated with the prevalence of MSP, such as age, ethnicity, occupation, number of children, and mode of delivery [11, 12]. Previous studies have implicated the breastfeeding position of lactating mothers as a contributor to MSP and its severity [8, 11, 12, 13].
Knowing the prevalence of MSP in a specific population and the preferred position associated with the location and intensity of MSP could help to decrease the burden of breastfeeding on a lactating mother’s body; it can also provide appropriate information to guide maternal education and help to prevent or decrease MSP [14]. The presence of pain affects breastfeeding outcomes, which has consequences for both maternal and infant health [15, 16]. Some mothers stop breastfeeding as a result of pain [17]. It is crucial to address and manage pain-related challenges to support and encourage mothers to continue breastfeeding. By doing so, we can ensure the well-being of both the mother and the baby, while reaping the numerous benefits associated with breastfeeding. Maternal education empowers women to be prepared and have accurate information about what to expect during breastfeeding, including teaching them how to position and hold a baby to ensure that there is successful milk latching with minimal pain or discomfort [18, 19, 20].
Therefore, the aims of this study were (1) to examine the prevalence of MSP; (2) to assess the MSP intensities in different body locations; and (3) to study the association between MSP location and breastfeeding positioning among lactating mothers in Riyad, Saudi Arabia.
This was a descriptive cross-sectional study using an online self-administered questionnaire. The study participants were recruited from hospitals and healthcare centres in the Riyadh Second Health Cluster (three hospitals and 48 health care centres) in Saudi Arabia. The questionnaires were distributed and collected over two months between October and December 2022.
The participants were lactating mothers aged 20–50 years, six weeks to one year after childbirth. Mothers were excluded if they had orthopaedic, neurological, or cardiovascular and respiratory conditions, multiple pregnancies, a preterm infant or infant with congenital anomaly, severe complications postpartum, or complained of MSP prior to pregnancy.
The minimum sample size required was calculated based on the following formula:
n = Z
A Google Forms platform was used to administer the questionnaires. The online questionnaire link was sent directly to each mother’s mobile number, which was collected from her medical file. In addition, an invitation barcode for the study was placed in the waiting area of hospitals and health care centres. Before starting answering the questions, the participant had to type her last 4 digits of her national identification number to eliminate multiple participation. In order to speed up the questionnaire, some negative responses were jumped to subsequent sections. Before moving on to the next section, a response was required. Answers could not be sent unless the questionnaire was completely filled out. A message thanking them appeared after answering the questions.
A self-administered questionnaire to collect the data was developed based on the literature. The face and content validity of the questionnaire were assessed by four experts (two physical therapists, one nurse, and one health educator), and 10 lactating mothers. The questionnaire consisted of three sections containing close-ended questions. The first section included eight questions related to sociodemographic and maternal characteristics (age group, education level, work status, number of children, mode of delivery, postpartum complications, multiple pregnancy, and preterm infant or infant with congenital anomaly), in addition to two questions related to receiving health education during pregnancy or after giving birth (general health education and expected musculoskeletal pain) and one question related to general health status (orthopaedic or neurological disorders prior to pregnancy).
The second section was related to the most assumed breastfeeding position. This section was accompanied by pictorial representations of the five most common breastfeeding positions (cradle position, cross-cradle position, side-lying position, football hold, and laid-back position).
The third section included body maps of six body sites (lower back, upper back,
neck, shoulders, arms, and hands) based on the Nordic pain questionnaire and six
questions related to the presence or absence of pain at each location during the
past 14 days that was present during or after breastfeeding. After each question
in this section, a Pain Intensity Numeric Rating Scale (PI-NRS) was added to
assess the pain intensity for each location. The PI-NRS is an 11-point pain
intensity scale, where zero indicates no pain and 10 represents the worst
possible pain. The pain intensity was categorized as mild if the PI-NRS scores
Electronic questionnaire data were automatically transferred to an Excel
spreadsheet, and then imported into a statistical program. IBM SPSS Statistics
for Windows (Version 28, IBM Corp., Armonk, NY, USA) was used for the analysis.
Descriptive statistics in terms of frequency and percentage were used to describe
the participants’ characteristics, breastfeeding positioning, MSP prevalence, and
pain intensity categories. The median and first and third interquartile range
(IQR) was used to describe the pain intensity ratings. Pearson’s chi-square test
(
A total of 400 responses were received; 64 were excluded because the mothers did not meet the inclusion criteria (59 were not active lactating mothers, and five had preterm infants). A total of 336 lactating mothers with ages ranging from 20 to 50 years (53.6% were aged between 31 and 40 years) were included in this study. More than half of the mothers reported mostly assuming the cradle position during breastfeeding (54.8%). Only 25% received education related to expected musculoskeletal pain during breastfeeding. The participant characteristics are presented in Table 1.
| Frequency | Percentage | ||
| Age group | 20–30 | 102 | 30.4% |
| 31–40 | 180 | 53.6% | |
| 41–50 | 54 | 16.1% | |
| Education level | High school or lower | 130 | 38.7% |
| Bachelor degree or higher | 206 | 61.3% | |
| Work status | Working mother | 153 | 45.5% |
| Number of children | First child | 13 | 3.9% |
| 1–4 children | 249 | 74.1% | |
| More than 4 children | 74 | 22.0% | |
| Mode of delivery | Vaginal | 196 | 58.3% |
| Caesarean section | 140 | 41.7% | |
| Health education received | General maternal education | 255 | 75.9% |
| Musculoskeletal pain | 84 | 25.0% | |
| Breastfeeding positions | Football position | 34 | 10.1% |
| Cross-cradle position | 49 | 14.6% | |
| Cradle position | 184 | 54.8% | |
| Side-lying position | 60 | 17.9% | |
| Laid-back position | 9 | 2.7% | |
A total of 327 (97.3%) mothers reported pain in at least one location on their bodies. The highest percentage of severe pain was reported for the lower back (19.1%), followed by neck pain (14.9%) (see Table 2 and Fig. 1). The median (and IQR in parentheses) of the pain intensity ratings for the different locations were as follows: lower back 4 (0, 6), upper back 2 (0, 5), neck 3 (0, 6), shoulders 3 (0, 5), arms 2 (0, 4), and hands 1 (0, 4). Lower back pain was the most frequent MSP (72.3%) and had the highest pain intensity rating of the lactating mothers.
| MSP | Prevalence | Pain intensity categories | ||
| Mild | Moderate | Severe | ||
| Lower back | 243 (72.3%) | 236 (70.2%) | 36 (10.8%) | 64 (19.1%) |
| Upper back | 224 (66.7%) | 263 (78.3%) | 45 (13.3%) | 28 (8.4%) |
| Neck | 227 (67.6%) | 251 (74.7%) | 35 (10.4%) | 50 (14.9%) |
| Shoulders | 211 (62.8%) | 262 (78.0%) | 39 (11.6%) | 35 (10.4%) |
| Arm | 197 (58.6%) | 286 (85.1%) | 43 (12.8%) | 7 (2.1%) |
| Hand | 197 (58.6%) | 288 (85.7%) | 42 (12.5%) | 6 (1.9%) |
Prevalence presented as frequency and percentage; N, number of participants; MSP, musculoskeletal pain.
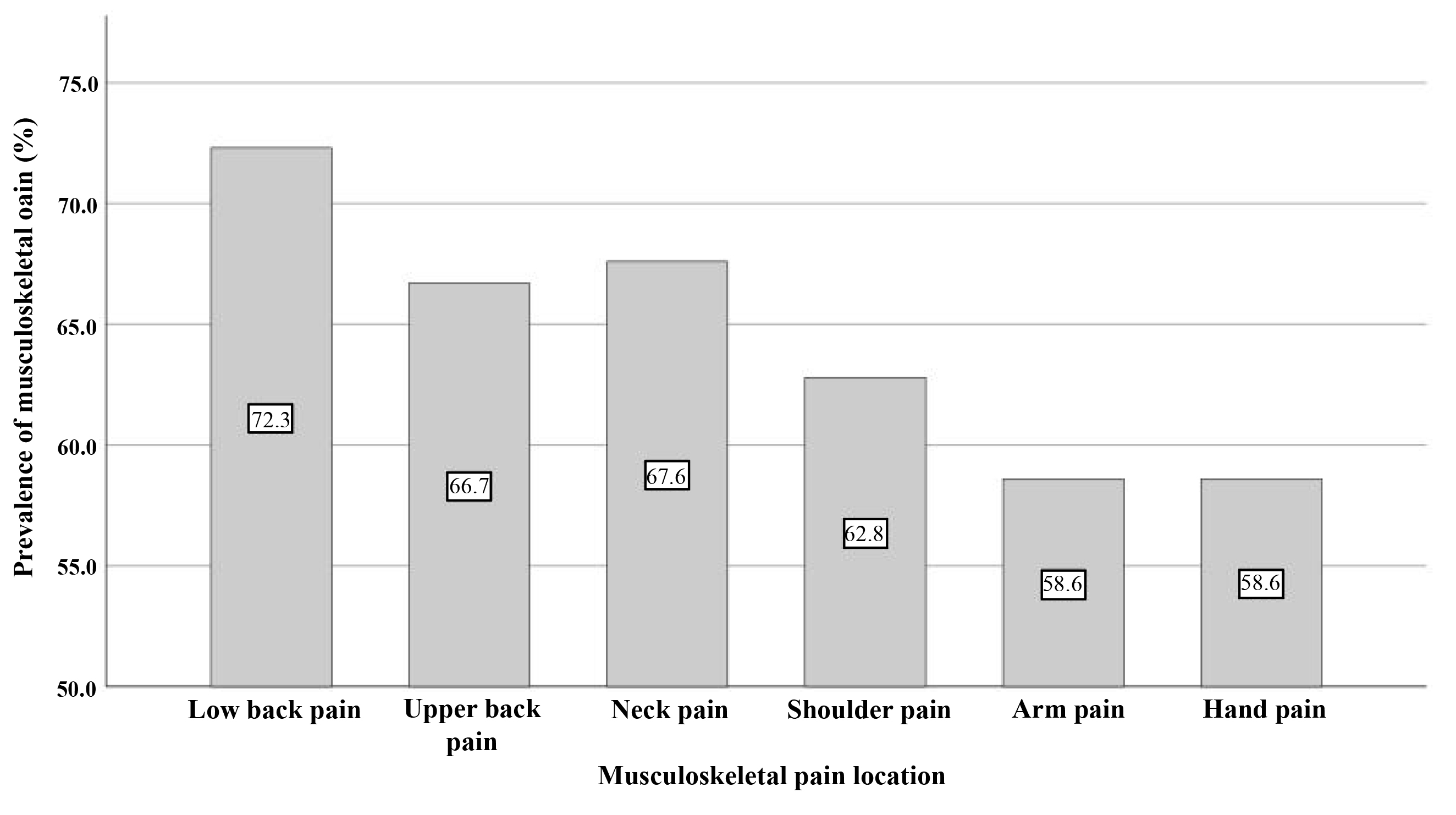 Fig. 1.
Fig. 1.Prevalence of musculoskeletal pain.
The MSP score was significantly correlated with different breastfeeding position
(p
| MSP | Prevalence respective to breastfeeding position | |||||||
| Football | Cross-cradle | Cradle | Side lying | Laid back | df | p | ||
| Lower back | 26 (10.70%) | 19 (7.82%) | 151 (62.14%) | 45 (18.52%) | 2 (0.82%) | 48.07 | 4 | |
| Upper back | 26 (11.6%) | 5 (2.23%) | 153 (68.30%) | 32 (14.29%) | 8 (3.57%) | 101.07 | 4 | |
| Neck | 24 (10.57%) | 30 (13.22%) | 146 (64.32%) | 27 (11.89%) | 0 (0%) | 45.38 | 4 | |
| Shoulders | 32 (15.17%) | 17 (8.06%) | 143 (67.78%) | 31 (14.69%) | 1 (0.47%) | 62.76 | 4 | |
| Arm | 31 (15.74%) | 5 (2.53%) | 131 (66.50%) | 23 (11.68%) | 7 (3.55%) | 85.75 | 4 | |
| Hand | 31 (15.74%) | 5 (2.53%) | 131 (66.50%) | 23 (11.68%) | 7 (3.55%) | 85.75 | 4 | |
Prevalence presented as frequency and percentage; N, number of participants; MSP,
musculoskeletal pain;
The number of previous births (number of children) showed no correlation with MSP in low back (p = 0.57), upper back (p = 0.40), neck (p = 0.23), shoulder (p = 0.97), arm (p = 0.12), or hand (p = 0.12). Additionally, it showed no correlation with breastfeeding position (p = 0.06).
This study assesses the prevalence of musculoskeletal pain and its association
with breastfeeding positioning in lactating mothers in Saudi Arabia.
Approximately 97.3% of lactating mothers complained of MSP. Lower back pain was
the most prevalent and intense pain (72.3% and median = 4, respectively),
followed by neck pain (67.6% and median = 3, respectively). Most of the mothers
adopted a cradle position during breastfeeding (54.8%). MSP was significantly
associated with breastfeeding position (p
In previous studies, similar results were reported in different populations; a high prevalence of MSP was reported by Indian and Pakistani mothers (99% and 74%, respectively) [6, 8]. In line with other studies, lower back and neck pain were the most common sites of MSP [6, 7, 8, 11, 12].
The cradle position was the most common for the lactating process among mothers, which was consistent with other studies [7, 11, 12]. This position can cause the pectoral girdle, along with the pelvic girdle, to experience stress as the mother leans forward to reach the infant’s mouth [9, 24], which could explain the high prevalence of lower back and neck pain. The laid-back position, despite being uncommon, was found to have the least correlation with pain in this study. This position naturally provides support and alignment for the back, head, and neck during breastfeeding. This finding further emphasizes the significance of adopting ergonomic positioning while nursing [25].
In agreement with Rani et al. [8], there was a significant association between MSP and breastfeeding position. Unlike the current study, those researchers found more MSP in the neck than in the lower back. In addition, in their study, cross-cradle was the most common position in which the mother supported the infant’s head with the hand opposite the feeding breast; thus, in addition to forward leaning, some rotation of the upper body, including the neck, was involved [8, 9, 24]. This could explain why most of the mothers reported neck pain during breastfeeding. The results of this study contradict a previous study carried out in Malaysia in which no correlation between breastfeeding position and neck pain was found [11]. However, in the current study, we examined the association of MSP in different locations with breastfeeding position, while in their study, they only looked at the correlation of MSP with neck pain.
There was variation in the pain intensity reported by the mothers. This was
similar to a study conducted among Indian mothers [6] in which the average pain
intensity using a similar pain scale indicated mild pain (3.63
Interestingly, 75% of the mothers reported receiving health education during pregnancy or after giving birth, but only 25% received health education related to breastfeeding MSPs. It was taught to them that musculoskeletal pain can occur during breastfeeding, so they should stay in a comfortable position to prevent it. These instructions do not cover proper posture, proper positioning, proper use of equipment like pillows and cushions, and how to avoid pain. This could be a reason for the high prevalence of MSP. This finding contrasted with previous research; for example, researchers found that most Jordanian lactating mothers were not educated on breastfeeding positioning or safe practices [24]. Moreover, another study showed that there was a lack of knowledge and practice of appropriate breastfeeding positions among Nigerian lactating mothers, which could be the cause of MSP [26]. An additional study found that mothers could benefit from ergonomic training by improving their knowledge, which would affect their behaviour and posture during breastfeeding and decrease the risk of MSP [27].
Because this study was limited to one city, the results cannot be generalized to other regions. We have not considered other factors that might have contributed to musculoskeletal pain, such as age and weight of babies, sociodemographic and psychological factors (such as post-partum depression), which can influence MSP. In addition, we did not examine whether mothers breastfed while sitting in a chair or on the floor. We also did not examine if they provided body support (for their backs, arms, or feet) during breastfeeding. Future studies are suggested to evaluate the relationship between these types of factors and musculoskeletal pain, examine the disability that could result from MSP, and find ways to raise mothers’ awareness levels of MSP and good breastfeeding practice. Moreover, mothers experiencing persistent nipple pain or deep breast pain should be evaluated for musculoskeletal pain [28].
In order to improve patient outcomes and improve the overall quality of care provided, it is crucial to address the lack of medical education on MSP and nursing positioning. Healthcare professionals can provide optimal care, improve mothers’ comfort, and facilitate better recovery by recognizing the importance of physiotherapy in these disciplines and implementing effective strategies to bridge the education gap. Physiotherapy and nursing positioning must be integrated into medical institutions’ educational programs to achieve well-rounded post-partum care.
Despite limited health education on MSP received by the mothers, MSP is prevalent among breastfeeding mothers in Riyadh, Saudi Arabia, especially lower back and neck pain. MSP was significantly associated with breastfeeding position, notably the cradle position, but less frequently with the Semi-reclined position. it is important to recognize that in the end, an ergonomic breastfeeding positioning that provides spinal alignment and back and neck support could be more important than the breastfeeding position itself.
The data that support the findings of this study are available upon request from the corresponding author. The data are not publicly available due to their containing information that could compromise the privacy of the research participants.
Both of the listed authors made substantial contributions to this manuscript. AA and MA contributed to the conception and design of the study, collected the data, participated in the data analysis and writing of the first draft of the manuscript, and in the writing process and preparation of the final version of the manuscript. Both authors provided critical feedback and helped shape the research, analysis, and manuscript; and approved the final version of the manuscript. Both authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
Ethical approval was obtained from the Institutional Review Board of King Fahad Medical City (IRB Log Number: E-22-7446). A brief description of the study, the estimated completion time, and the contact information for the principal investigator were included at the beginning of the survey. By choosing to complete the survey, participants provided their consent. The privacy of the participants’ information was maintained, and there was no disclosure of their names or any information that could identify them.
We are grateful to all the mothers who participated in this study.
This research received no external funding.
The authors declare no conflict of interest.
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
