- Academic Editor
Background: The purpose of this study was to compare the effect of pre- and post-treatment furosemide on reducing intravascular absorption syndrome in complex hysteroscopic leiomyoma surgery. Methods: This randomized controlled study enrolled 62 patients who underwent hysteroscopic leiomyoma surgery in Fuxing Hospital, Capital Medical University. Patients were randomly allocated to pre- and post-treatment furosemide groups. Information on patient age, body mass index, sum of the three diameters of the uterus, sum of diameter of submucosal myoma, and intimal thickness were recorded. The mean arterial pressure and heart rate were recorded at entry to the operating room, after anesthesia induction, at the end of operation, and after laryngeal mask pulled out. The duration of anesthesia, recovery time after withdrawal of anesthetic drug, amount of sufentanil, amount of propofol, amount of uterine perfusion fluid, the amount of perfusion fluid flowing out, the actual amount of fluid intake, the proportion of pulmonary diffuse B-line in perioperative period, and uterine perfusion pressure during operation were also recorded, together with postoperative adverse reactions (drowsiness, nausea, vomiting, chills). Results: No significant differences were observed between the pre- and post-treatment groups in terms of patient age, body mass index, sum of the three diameters of the uterus, sum of diameter of submucosal myoma, and intimal thickness. The mean arterial pressure and heart rate at the four different time points were not significantly different between the two groups, nor were there any significant differences in the duration of anesthesia, the amount of sufentanil, the amount of propofol, the amount of intrauterine perfusion fluid, the amount of perfusion fluid flowing out, the actual amount of fluid intake, the intrauterine perfusion pressure, or the incidence of postoperative drowsiness, nausea and vomiting. However, pre-treatment with furosemide was associated with a significantly reduced recovery time (p = 0.037) and incidence of postoperative chills (p = 0.032) compared to the post-treatment group. Furosemide significantly reduces the number of B-lines. Conclusions: Furosemide preconditioning can reduce the recovery time and occurrence of postoperative chills, both of which are conducive to better postoperative recovery. Clinical Trial Registration: The study was registered at https://www.chictr.org.cn (registration number ChiCTR2200062840).
Hysteroscopic surgery is a minimally invasive gynecological diagnosis and treatment technique. It is widely used in the clinic because it has the advantages of minimal trauma, quick recovery, and short hospital stay for postoperative recovery. Leiomyomas are the most common pelvic tumors, while submucosal fibroids are a common cause of abnormal bleeding and infertility [1]. OHIAS refers to a series of complications, such as pulmonary edema and heart failure, that result from fluid overload caused by large amounts of dilatant fluid entering the blood during hysteroscopic surgery. Due to the long duration, high perfusion pressure, and large perfusion flow of complex hysteroscopic surgery, a large amount of liquid is absorbed into the patient’s circulatory system through the intrauterine venous sinus and salpingot-peritoneum [2]. This leads to OHIAS, which in severe cases can directly endanger the patient’s life and safety. A 2020 expert consensus on anesthesia management in hysteroscopic diagnosis and treatment in China found the most common complications of hysteroscopic surgery were uterine perforation (0.12%), OHIAS caused by excess distention fluid (0.06%), intraoperative bleeding (0.03%), air embolism syndrome (0.03%), bladder or intestinal injury (0.02%), and endometritis (0.01%) [3]. The relatively high incidence of uterine perforation and OHIAS was noted with concern.
Currently, the prevention of OHIAS usually involves reducing uterine pressure, shortening the operation time, and reducing the amount of dilation fluid into the uterus [4]. Individual differences exist for the safe threshold of dilation fluid intake, with a threshold range of approximately 750 mL to 1000 mL for the electrolyte free solution depending on the patients’ body weight, cardiopulmonary function and other complications [5]. As for the normal saline, the safe threshold of fluid intake is 2500 mL [6]. Although many rules have been formulated and implemented for hysteroscopic surgery, the risks of pulmonary edema and heart failure still exist due to the increased circulating blood volume caused by large amounts of perfusion fluid entering the circulatory system during surgery [7]. Therefore, the monitoring of changes in lung fluid and preconditioning at the right time are crucial for reducing postoperative complications.
Ultrasonic monitoring of the lungs can accurately assess the condition of lung fluid. This is well established, performed routinely, and not limited by the time, place or cost of the procedure [8, 9, 10]. Lung B ultrasound conducted with an ultrasound probe shows imaging characteristics based on the different “air/water” ratios of lung tissue. Line A indicates the lung tissue is normal, whereas line B indicates the lungs are full of water. Thus, an increasing B line indicates gradually increasing pulmonary fluid [11]. During B-ultrasound examination, each side of the chest wall is divided into four zones, with a total of eight zones on both sides. The left side of the lung scan is from the second rib to the fourth rib, and the right side is from the second rib to the fifth rib. The sensor probe is scanned along the parasternal, mid-clavicle, anterior axilla and midaxillary line, thereby recording all B lines in the eight zones [12, 13]. The recognized positive index for B-ultrasound to indicate pulmonary edema is three or more B-lines in any two areas at the same time [10].
In the present study, B-ultrasound was used to monitor changes in lung water. Intravenous furosemide was administered when positive indicators of pulmonary edema appeared. The perioperative effects of pre- and post-treatment with furosemide were then compared. The aim was to determine the optimal time point for preconditioning in order to prevent pulmonary edema during hysteroscopic leiomyoma surgery. This could provide anesthesiologists with a strategy to prevent pulmonary edema during surgery, thus also reducing the probability of complications.
The doctors who conducted B-ultrasound monitoring in this study had received more than 6 months of professional training in pulmonary ultrasound monitoring.
This study was a randomized controlled clinical trial conducted in Fuxing Hospital, Capital Medical University, China. The study was approved by the institutional ethics committee (trial registration: 2022FXHEC-KY003), and all subjects signed informed consent. The study was registered at https://www.chictr.org.cn (registration number ChiCTR2200062840).
The inclusion criteria were: (1) age 20–60 years; (2) American Society of
Anesthesiologists (ASA) grade 1–2; (3) patient scheduled for hysteroscopic
surgery, with furosemide being used during surgery; (4) submucosal myoma
(diameter
A total of 62 patients who received hysteroscopic surgery in the Hysteroscopic Center of Fuxing Hospital, Capital Medical University from March 2022 to December 2022 were randomly divided into two groups using a computer-generated random number table. The numbers were sealed in envelopes and later opened by the main investigator to assign the allocated treatment. Eligible patients were allocated to the furosemide post-treatment group (n = 31) or to the furosemide pre-treatment group (n = 31). The process for assigning participants to each group is shown in a flow chart in Fig. 1. Patients and surgeons were blind to the assigned group.
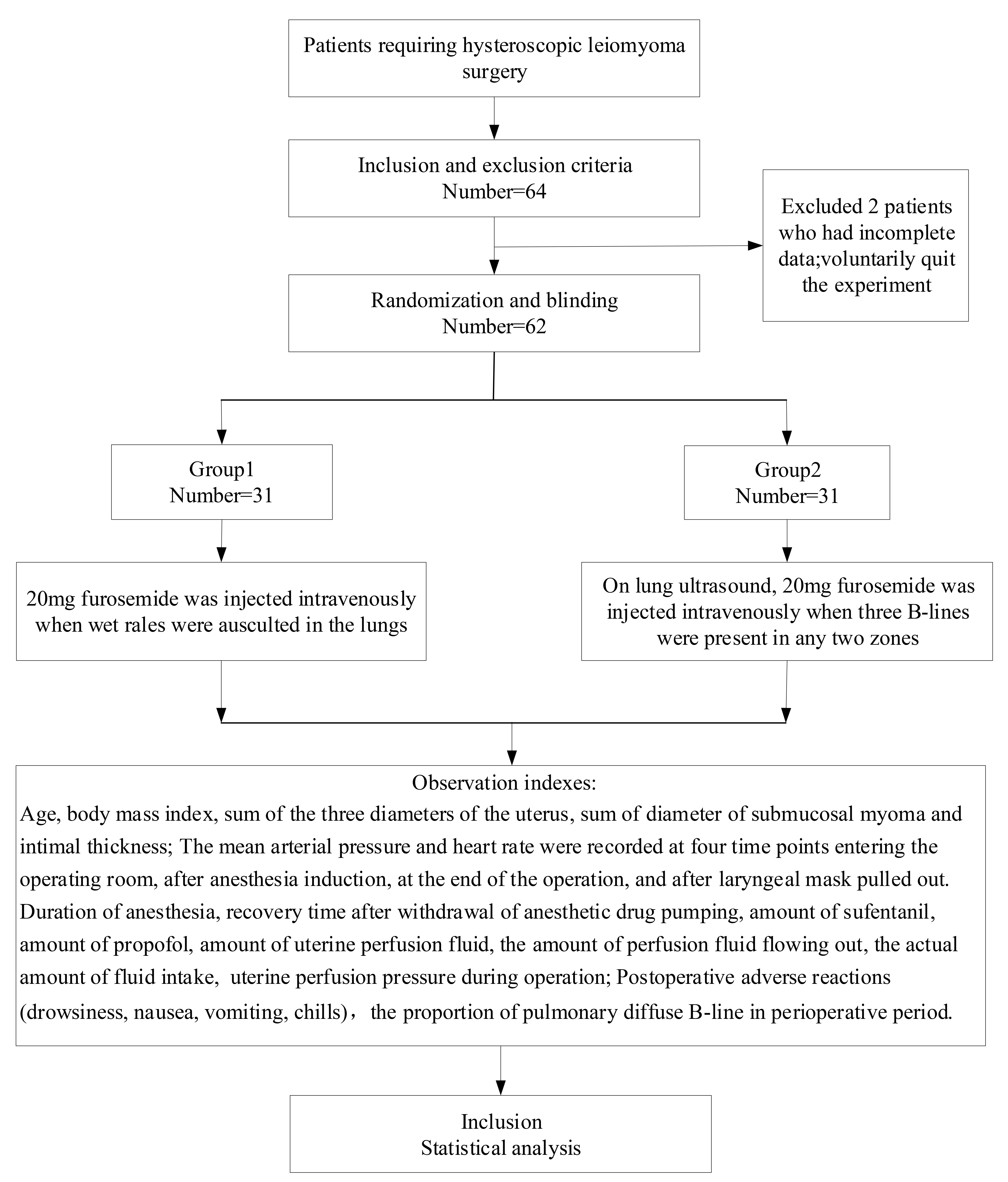 Fig. 1.
Fig. 1.Flow chart.
Group 1: 31 cases in the furosemide post-treatment group; 20 mg of intravenous furosemide when the lung auscultation was a wet rales sound.
Group 2: 31 cases in the furosemide pre-treatment group; the change in pulmonary water was monitored by ultrasound scanning during operation, and 20 mg of furosemide was injected intravenously when three B lines appeared simultaneously in any two zones.
During induction, the two groups received sufentanil (0.2 µg/kg) and propofol initiated at 6 µg/mL via target-controlled infusion (TCI). The two groups then received continuous propofol during the maintenance phase, with the dosage adjusted to maintain the bispectral index (BIS) at 45–55. The monitor used was an Infinity Vista XL (Dräger, Lubeck, Germany), and the anesthesia machine was a Fabius 2000 (Dräger, Lubeck, Germany).
All other procedures were the same in both groups. The end-expiratory carbon dioxide partial pressure was maintained at 35–45 mmHg during operation, with BIS maintained at 45–55.
Hysteroscopic leiomyoma surgery is a minimally invasive surgery. The uterine orifice was fully expanded and physiological salt was pumped into the uterine cavity at 70–80 mmHg pressure prior to the hysteroscopic operation. Pathological examination of the specimens confirmed they were uterine fibroids.
In both groups, patient data was recorded for age, body mass index, sum of the three diameters of the uterus, sum of the diameter of submucosal myoma, and intimal thickness. The mean arterial pressure and heart rate were recorded at four time points: entry into the operating room, after anesthesia induction, at the end of operation, and after laryngeal mask pulled out. Also recorded for each patient were the duration of anesthesia, recovery time after withdrawal of anesthetic drug, amount of sufentanil administered, amount of propofol administered, amount of uterine perfusion fluid, the amount of perfusion fluid flowing out, the actual amount of fluid intake (the difference between the amount of infusion and outflow), and the uterine perfusion pressure during operation. Postoperative adverse reactions (drowsiness, nausea, vomiting, chills), the proportion of pulmonary diffuse B-line in perioperative period (Intercostal space 50% line B) were also noted.
SPSS 26.0 (IBM Corp., Armonk, NY, USA) was used for statistical analysis.
Continuous variables that conformed to a normal distribution (Kolmogorov-Smirnov
test) were presented as the mean
A total of 62 patients were enrolled in the study, with 31 cases in each group (Fig. 1). Surgery was successful in all patients. No statistically significant differences were observed between the two groups for patient age, body mass index, sum of the three diameters of the uterus, sum of the diameter of submucosal myoma, and intimal thickness. Furthermore, no significant differences between the two groups were seen for the mean arterial pressure and heart rate at the four time points at which these were assessed (Table 1).
| Characteristics | All (n = 62) | Group 1 (n = 31) | Group 2 (n = 31) | t | p |
| Age (years) | 36.8 |
35.6 |
38.0 |
1.232 | 0.223 |
| BMI (kg/m |
22.2 |
22.4 |
22.0 |
0.494 | 0.623 |
| Sum of uterus diameters (mm) | 170.1 |
168.2 |
172.1 |
0.439 | 0.662 |
| Sum of submucosal myoma diameter (mm) | 89.3 |
98.9 |
78.4 |
1.754 | 0.085 |
| Intimal thickness (mm) | 5.1 |
5.5 |
4.7 |
0.857 | 0.395 |
| Mean entry arterial pressure (mmHg) | 92.4 |
92.4 |
92.5 |
0.024 | 0.981 |
| Mean arterial pressure after induction (mmHg) | 79.9 |
77.3 |
82.6 |
1.804 | 0.076 |
| Mean arterial pressure at the end of surgery (mmHg) | 84.2 |
83.9 |
84.5 |
0.168 | 0.867 |
| Mean arterial pressure after laryngeal mask pulled out (mmHg) | 86.2 |
85.8 |
86.7 |
0.329 | 0.743 |
| Heart rate of invasion (bpm) | 73.4 |
73.3 |
73.6 |
0.139 | 0.890 |
| Post-induction heart rate (bpm) | 67.8 |
65.9 |
69.7 |
1.651 | 0.104 |
| End of operation heart rate (bpm) | 65.6 |
64.4 |
66.8 |
0.926 | 0.358 |
| Heart rate after extubation (bpm) | 68.5 |
69.2 |
67.9 |
0.458 | 0.649 |
BMI, body mass index; SD, standard deviation.
No significant differences were observed between the two groups for the duration of anesthesia, amount of sufentanil, amount of propofol, amount of uterine perfusion fluid, the amount of perfusion fluid flowing out, the actual amount of fluid intake, or uterine perfusion pressure. However, there was a statistically significant difference in the recovery time between the two groups (p = 0.037) after withdrawal of the anesthetic drug (Tables 2,3).
| Characteristics | All (n = 62) | Group 1 (n = 31) | Group 2 (n = 31) | t | p |
| Anesthesia time (min) | 60.6 |
60.8 |
60.3 |
0.148 | 0.883 |
| Recovery time (min) | 5.3 |
5.9 |
4.7 |
2.129 | 0.037* |
SD, standard deviation.
*: Group 2 is compared with group 1, p
| Characteristics | All (n = 62) | Group 1 (n = 31) | Group 2 (n = 31) | Wilcoxon test | |
| z | p | ||||
| Sufentanil (µg) | 15 (10, 15) | 15 (10, 15) | 12 (10, 17.5) | 0.367 | 0.714 |
| Propofol (mg) | 60 (55, 70) | 60 (52.5, 67.5) | 60 (55, 72.5) | 1.437 | 0.151 |
| Perfusion pressure (cmH |
120 (120, 120) | 120 (120, 120) | 120 (120, 120) | 0.116 | 0.908 |
| Intrauterine perfusion volume (mL) | 10,000 (9000, 12,000) | 10,000 (9000, 12,000) | 11,000 (9500, 12,000) | 1.149 | 0.250 |
| The amount of perfusion fluid flowing out (mL) | 7200 (1000, 13,000) | 7000 (2000, 12,900) | 7600 (1000, 10,000) | 1.120 | 0.263 |
| The actural amount of fluid intake (mL) | 3000 (2000, 4400) | 2900 (2000, 4400) | 3000 (2000, 3500) | 0.605 | 0.545 |
IQR, interquartile range.
There were no significant differences in the incidence of drowsiness, nausea or vomiting between the two groups. However, the incidence of postoperative chills was significantly lower (p = 0.032) in the pre-treatment group, and the proportion of pulmonary diffuse B-line in perioperative period was significantly lower also in the pretreatment group (p = 0.016) (Table 4).
| Characteristics | All (n = 62) | Group 1 (n = 31) | Group 2 (n = 31) | p | |
| Drowsiness | 1 (1.6%) | 1 (3.2%) | 0 (0%) | 0.000 | 1.000 |
| Nausea | 3 (4.8%) | 1 (3.2%) | 2 (6.5%) | 0.000 | 1.000 |
| Vomit | 1 (1.6%) | 1 (3.2%) | 0 (0%) | 0.000 | 1.000 |
| Chills | 6 (9.7%) | 6 (19.4%) | 0 (0%) | 4.613 | 0.032 |
| The proportion of pulmonary diffuse B-line | 16 (21.5%) | 15 (48.4%) | 6 (19.4%) | 5.833 | 0.016 |
#,*: Group 2 was compared with group 1, p
The present study found that monitoring of changes in lung water and pre-treatment with furosemide can shorten the recovery time and reduce postoperative chills after complex hysteroscopic leiomyoma surgery.
OHIAS is known to cause massive perfusion of fluid into the uterus during hysteroscopic leiomyoma surgery. This manifests mainly as pulmonary edema and heart failure in severe cases, thus presenting a challenge for perioperative management by anesthesiologists. OHIAS can lead to a series of life-threatening complications, including pulmonary edema and brain edema. However, prompt diagnosis and early management can reduce the risk of developing serious complications [14]. Onk et al. [15] achieved good results in patients with negative pressure pulmonary edema by treating with intravenous diuretics. The present study showed that early treatment with furosemide in patients with acute pulmonary edema caused by excessive fluid was more effective at improving their symptoms and promoting recovery than later treatment. By reducing pulmonary edema, intravenous furosemide can therefore help patients to recover sooner, thus reducing the likelihood of postoperative complications such as dyspnea and agitation. In a study on the effectiveness of diuretics in treating pulmonary edema caused by heart failure, Khan et al. [16] reached the same conclusion as the present investigation. Oricco et al. [17] also found that oxygen therapy, continuous positive airway pressure, and furosemide therapy have a major positive impact on the survival of patients with pulmonary edema. In summary, furosemide is effective in the prevention of pulmonary edema arising from hysteroscopic leiomyoma surgery.
Ultrasonic monitoring of the lungs can accurately assess lung water condition and is therefore widely performed in clinical practice. Lo et al. [18] performed pulmonary ultrasound in patients with increased respiratory work and with a gradual decrease in oxygen saturation after surgery. Their results showed a large number of B-lines in multiple lung fields, consistent with pulmonary edema caused by excessive fluid. The patients in their study recovered after treatment with furosemide. Pulmonary ultrasound has a guiding role in the rapid bedside assessment and treatment of patients with pulmonary edema. It can also detect and diagnose pulmonary edema at an early stage. Our study showed that preconditioning with furosemide based on the presence of three B-lines in lung ultrasound can accelerate postoperative recovery and reduce the incidence of postoperative chills. Deng et al. [19] showed that furosemide can help to reduce transurethral resection during hysteroscopic leiomyoma surgery, thereby preventing neurological sequelae and other serious problems from arising. Griva et al. [20] reported that furosemide could prevent fluid overload and reduce the occurrence of pulmonary edema. The results of their study also agree with the present findings. Therefore, early treatment with furosemide can prevent intravascular absorption syndrome caused by hysteroscopic leiomyoma surgery.
The present study had several limitations. First, it was a single-center study and hence multi-center studies should be carried out in different regions and for different ethnic groups. Second, the sample size should be expanded in future studies.
In conclusion, pre-treatment with furosemide following the monitoring of changes in lung water can shorten the recovery time and reduce postoperative chills in patients undergoing complex hysteroscopic leiomyoma surgery, thereby improving their recovery.
All data generated and analyzed during this study are included in the published article.
XC—data collection, extraction, drafting of the manuscript, analysis of data, manuscript revision; XD—data collection; HHS—data collection; XYW—analysis of data. All authors contributed to editorial changes in the manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work. All authors read and approved the final manuscript.
All subjects gave their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of Fu Xing Hospital, Capital Medical University (approval number: 2022FXHEC-KY003).
We would like to express my gratitude to all those who helped me during the writing of this manuscript.
This study was supported by Beijing Xicheng District Health Commission Young Science and Technology Talents (Science and Technology Nova) Training Program (#XWKX2022-21).
The authors declare no conflict of interest.
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
