- Academic Editor
Background: To determine the value of the uterocervical angle for
predicting the displacement of copper intrauterine devices (IUDs).
Methods: We conducted a prospective cohort study between December
2020–June 2021 at the family planning outpatient clinics of the Kanuni Sultan
Suleyman Training and Research Hospital, Istanbul Health Sciences University. A
total of 143 patients who had copper IUDs (T-Cu380A) inserted for contraception
were evaluated from the 6th week to 5 years after insertion. Patients were
divided into two groups according to ultrasonographic examinations that revealed
whether their IUD were “displaced” or in the “normal” position. The
uterocervical angle (UCA) of patients was measured by transvaginal
ultrasonography and investigated as to whether it was predictive for the
displacement of copper IUDs. Results: Of the 143 women participating in
the study, 67 (46.9%) had a displaced IUD position, and 76 (53.1%) had a normal
IUD position. No statistically significant difference was found between the two
groups for patient age, body mass index, educational status, gravida, parity, and
mode of delivery (p
Family planning uses several methods of protection, one of which is copper intrauterine devices (IUDs). This has become a favored contraception method due to its long-acting effect, rapid return to fertility once discontinued, and ease of use. Worldwide, IUDs are the third most common method of contraception after tubal ligation and male condoms [1]. Comparison of long-acting contraception methods revealed a failure rate for copper IUDs of 0.8% per year [2]. Factors that affect the displacement of IUDs are the application time [3], application technique [4], uterus dimensions [5], endometrial cavity length [6], parity [7], and mode of delivery [8]. Displacement of an IUD from its usual position at the fundal segment of the uterus is known to decrease its contraceptive efficacy. The above-mentioned factors causing copper IUD displacement can reduce the effectiveness of these devices, thereby increasing the possibility of unplanned pregnancy.
The displacement of copper IUDs triggers uterine contraction and forces foreign body expulsion from the endometrial cavity through the cervix. Several studies have explored the function of the uterine cervix by measuring the uterocervical angle (UCA) and the cervical length using ultrasonography [9, 10]. UCA is the angle in the triangular region between the anterior uterine segment and the cervical canal [9]. It has been used to predict the risk of preterm birth, embryo transfer success, and the severity of primary dysmenorrhea [9, 10, 11]. The UCA could play a role in the downward expulsion of copper IUDs during ill-fitting positions because it represents the relationship between the cervix and the endometrial cavity. This angle might influence the position of copper IUDs in the uterine border by applying a negative force against uterine contraction. The aim of the current research was therefore to investigate whether there is a cause-effect relationship between the utero-cervical junction and the displacement of copper IUDs. Thus, we studied the utility of UCA measurements for predicting the displacement of copper IUDs.
Included in this study were female patients aged 21–45 years who applied to our family planning outpatient clinic between January 2021 to June 2021 for control visits or attending with any complaints. We only included patients who were referred to our family outpatient clinic for IUD insertion earlier and then attended their follow-up visits. Follow-up visits were scheduled in the 6th week, at 6 months, and then annually after the first year until the 5th year (Fig. 1). Patients were divided into two groups either coming to their routine control visit and having a normal IUD position or referring to our outpatient clinic with various complaints due to IUD usage and having a dislocated IUD during ultrasonographic evaluation. Exclusion criteria were: hospital admission within 6 weeks of insertion, IUD insertions outside of our hospital, space-occupying lesions (polyps, myomas), pelvic inflammatory diseases, cervical polyps, uterine myomas, adenomyosis, uterine anomalies, connective tissue diseases, descensus uteri, abnormal uterine bleeding, immune suppression, anticoagulant usage, copper allergy or copper metabolism disorders (Wilson disease), or previous treatment for Atypical Squamous Cells of Undetermined Significance (ASCUS), Low-grade squamous intraepithelial lesion (LSIL), High-grade squamous intraepithelial lesion (HSIL), Cervical intraepithelial neoplasia (CIN) lesions or malignancy by any method (cryotherapy, Loop electrosurgical excision procedure (LEEP) or cone biopsy).
 Fig. 1.
Fig. 1.A flow-chart diagram illustrating patient selection and scheduled visits during 5 years of period. IUD, Intrauterine device; PAP-Smear, Papanicolaousmear.
IUD insertions were performed by the same certified and trained midwife (SS) at the Family Planning Center, Health Sciences University Istanbul, Kanuni Sultan Suleyman Training and Research Hospital (Turkey). IUD insertions in our family planning outpatient clinic are performed on the 3rd day of the menstrual period, at the 6th week postpartum, and at the 6th week post-cesarean. On rare occasions we also inserted IUDs after menstrual regulation, after dilatation curettage, and after cesarean section. Patients were informed of the risks of IUD expulsion at each time period, and IUDs were initiated based on their personal preference. Gynecological examinations and The Papanicolaou-smear screening were performed prior to IUD insertion. After insertion, transvaginal ultrasonography (TV-USG) was performed to confirm the correct IUD placement. Follow-up visits were scheduled in the 6th week, at 6 months, and then annually after the first year. Speculum examination and TV-USG was performed on all patients at each follow-up visit. Patients were questioned for the presence of symptoms related to IUD use. Demographic characteristics, type of delivery, the last delivery time, insertion time, education status, gynecological symptom history (chronic pelvic pain, menorrhagia, dysmenorrhea, dyspareunia, leukorrhea), hygiene habits (vaginal douche), menstrual pattern, medical history and previous IUD displacement were documented. The presence of IUD thread, leukorrhea, vaginal bleeding, or foul-smelling discharge was investigated by examination of the speculum.
TV-USG was performed to ascertain the device position. Ultrasounds were
performed vaginally using an ultrasound instrument (Aloka Prosound 6, 2008,
Tokyo, Japan) with a 3.5 MHz vaginal transducer. Patients were examined in the
lithotomy position and were asked to empty their bladder before examination. All
measurements were performed by a single physician (OK) in order to ensure the
standardization of ultrasonographic parameters and to minimize inter- and
intra-observer variation. Measurements included the uterus position (anteversion,
retroversion, anteflexion, retroflexion), cervical length, uterocervical angle
(UCA), fundal length (FL), endometrial cavity length (ECL), the distance behind
the intersection of the uppermost vertical arm of the IUD and the fundal
endometrium (IUD-End), and uterine volume (cm
 Fig. 2.
Fig. 2.A schematic illustration of ultrasonographic uterine measurements. (A) Schematic illustration of the distance between the top of the intrauterine device (IUD) and the end of the endometrial cavity (IUD-End). (B) Schematic illustration of the ultrasonographic parameters defined for the uterus. A–B: IUD-fundus length (FL); B–C: endometrial cavity length (ECL); C–D: cervical length (CX); uterocervical angle (UCA); total uterine length (TUL): FL + ECL + CX [(A–B) + (B–C) + (C–D)].
The UCA is the angle measured in the triangular region between the anterior uterine segment and the cervical canal. For measurements made in the sagittal section, the first line forming the angle was drawn between the external os and the internal os along the endocervical canal. If the cervical canal was not linear, this first line was determined as the straight line drawn between the internal os and the external os. The secondary line forming the UCA was determined as the straight line extending from the beginning of the internal os to the top of the fundus along the anterior uterine segment [10].
Measurements of the uterine cervical longitudinal axis were performed after the
image was enlarged to cover 3/4 of the screen. The internal cervical ostium,
external cervical ostium, cervical canal, and endocervical mucosa were viewed
simultaneously [11]. Three different images were obtained during the examination
of each patient, and the ideal and shortest cervical length were recorded.
Uterine volume was measured as follows: the uterine length was first calculated
from the fundus to the internal os with a vaginal probe on a sagittal plane. The
transducer was then moved 90° towards the transverse plane and adjusted
to give the maximum anteroposterior diameter. Following this, the anteroposterior
and transverse diameters were measured. Volume was calculated using the formula
for a prolate ellipsoid: Volume = (0.52
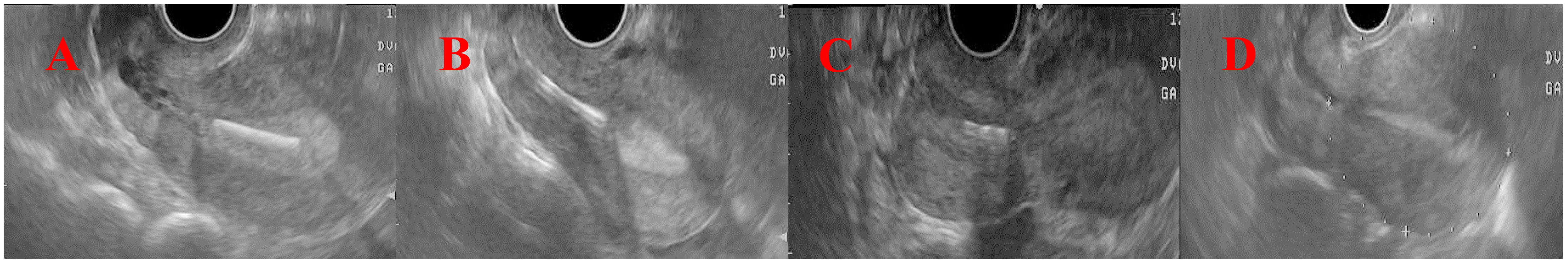 Fig. 3.
Fig. 3.Illustration of abnormal copper intrauterine device
positions. (A) Group 1: patients whose IUD fundus distance was
Statistical analyses were performed using SPSS v.21 (SPSS Inc., Chicago, IL,
USA). The distribution of variables was tested for normality using histograms and
the Kolmogorov Smirnov and Shapiro-Wilk W tests. Parametric continuous data are
presented as the mean
A total of 143 patients were enrolled in this study. Patients were categorized according to the position of their IUD as detected by ultrasonography during their 6-week follow-up visit after insertion. IUD displacement was observed in 67 patients (displaced group), while no IUD displacement was seen in 76 patients (control group). The mean age, body mass index (BMI), median parity, delivery type, timing of insertion, and IUD insertion time were not significantly different between these two groups. A comparison of the demographic characteristics of the two patient groups is shown in Table 1.
| Parameter | Displaced (n = 67) | Control (n = 76) | p-value | |
| Age (years) Mean |
33.2 |
33.7 |
0.661 | |
| BMI (kg/m |
27.5 |
26.4 |
0.158 | |
| Education n (%) | ||||
| No education | 9 (13.4) | 13 (17.1) | 0.889 | |
| Primary school | 26 (38.8) | 26 (34.2) | ||
| Secondary school | 19 (28.4) | 21 (27.6) | ||
| High school | 9 (13.4) | 13 (17.1) | ||
| University or PhD | 4 (6) | 3 (3.9) | ||
| Gravida Mean (IQR) | 3 (2–4) | 3 (2–4) | 0.296 | |
| Parity Mean (IQR) | 3 (2–4) | 2 (2–3) | 0.115 | |
| Abortion Mean (IQR) | 0 (0–0) | 0 (0–0.75) | 0.769 | |
| Curettage n (%) | ||||
| No | 58 (86.6) | 67 (88.2) | 0.775 | |
| Yes | 9 (13.4) | 9 (11.8) | ||
| Route of previous delivery n (%) | ||||
| Vaginal | 45 (67.2) | 42 (55.3) | 0.445 | |
| CS | 13 (19.4) | 23 (30.3) | ||
| Nulliparous | 1 (1.5) | 1 (1.3) | ||
| Vaginal + CS | 8 (11.9) | 10 (13.2) | ||
| Duration of IUD use n (%) | ||||
| 13 (19.4) | 17 (22.4) | 0.816 | ||
| 6–12 months | 11 (16.4) | 10 (13.2) | ||
| 43 (64.2) | 49 (64.5) | |||
| Timing of IUD insertion n (%) | ||||
| Postpartum 6th week | 48 (71.6) | 44 (57.9) | 0.077 | |
| 6 weeks after cesarean | 16 (23.9) | 26 (34.2) | ||
| After menstrual regulation | 3 (4.5) | 1 (1.3) | ||
| After D&C | 0 (0) | 3 (3.9) | ||
| After cesarean | 0 (0) | 2 (2.6) | ||
n (%), Number (Percentage); SD, Standard deviation; BMI, Body mass index; CS, Cesarean section; IUD, Intrauterine device; IQR, Inter quantile range; PhD, Doctorate of Philosophy; D&C, Dilatation and curretage.
The clinical characteristics of patients are shown in Table 2. Patients with
displaced IUDs showed more frequent menorrhagia (43% vs. 25%,
p = 0.021) and irregular menstrual pattern (51% vs. 22%,
p
| Parameters | Displaced (n = 67) | Control (n = 76) | p-value | |
| Length of menstrual cycle (days) Mean (IQR) | 7 (6–9) | 7 (5–8) | 0.230 | |
| Menstrual pattern n (%) | ||||
| Regular | 33 (49.3) | 59 (77.6) | ||
| Irregular | 34 (50.7) | 17 (22.4) | ||
| Menorrhagia history n (%) | ||||
| Yes | 29 (43.3) | 19 (25) | 0.021 | |
| No | 38 (56.7) | 57 (75) | ||
| Dyspareunia history n (%) | ||||
| Yes | 29 (43.3) | 30 (39.5) | 0.644 | |
| No | 38 (56.7) | 46 (60.5) | ||
| Dysmenorrhea history n (%) | ||||
| Yes | 34 (50.7) | 37 (48.7) | 0.806 | |
| No | 33 (49.3) | 39 (51.3) | ||
| Leukorrhea history n (%) | ||||
| Yes | 48 (71.6) | 58 (76.3) | 0.524 | |
| No | 19 (28.4) | 18 (23.7) | ||
| Vaginal douche history n (%) | ||||
| Yes | 25 (37.3) | 27 (35.5) | 0.825 | |
| No | 42 (62.7) | 49 (64.5) | ||
| Chronic pelvic pain n (%) | ||||
| Yes | 15 (22.4) | 17 (22.4) | 0.998 | |
| No | 52 (77.6) | 59 (77.6) | ||
Data are mean or n (%).
Table 3 shows the incidence of symptoms during presentation at follow-up. The
incidence of vaginal bleeding (28.4%) during speculum examination of patients
with IUD displacement was significantly higher than in patients without
displacement (5.3%) (p
| Displaced (n = 67) | Control (n = 76) | p-value | ||
| Leukorrhea n (%) | ||||
| Yes | 59 (88.1) | 58 (76.3) | 0.069 | |
| No | 8 (11.9) | 18 (23.7) | ||
| Vaginal bleeding n (%) | ||||
| Yes | 19 (28.4) | 4 (5.3) | ||
| No | 48 (71.6) | 72 (94.7) | ||
| Foul-smelling discharge n (%) | ||||
| Yes | 4 (6) | 6 (7.9) | 0.652 | |
| No | 63 (94) | 70 (92.1) | ||
| Missing IUD string (%) | ||||
| Yes | 6 (9) | 12 (15.8) | 0.219 | |
| No | 61 (91) | 64 (84.2) | ||
| Abdominal examination n (%) | ||||
| Normal | 61 (91) | 71 (93.4) | 0.743 | |
| Tenderness | 5 (7.5) | 5 (6.6) | ||
| Rigidity | 1 (1.5) | 0 (0) | ||
n (%), Number (Percentage).
The uterine characteristics of the two patient groups are compared in Table 4.
Patients with IUD displacement had significantly shorter cervical length
(p = 0.005), longer endometrial cavity length (p
| Uterine position/characteristics | Displaced (n = 67) | Control (n = 76) | p-value | |
| Uterine position 1 n (%) | ||||
| Anteverted | 51 (76.1) | 65 (85.5) | 0.378 | |
| Retroverted | 13 (19.4) | 9 (11.8) | ||
| Anterior midline | 3 (4.5) | 2 (2.6) | ||
| Uterine position 2 n (%) | ||||
| Anteflexed | 5 (7.5) | 6 (7.9) | 0.923 | |
| Retroflexed | 62 (92.5) | 70 (92.1) | ||
| Cervix length (mm) Mean |
28.7 |
30.2 |
0.005 | |
| Endometrial cavity length (mm) Mean |
48.8 |
41.4 |
||
| Fundal length (mm) Mean |
13.7 |
13.7 |
0.992 | |
| Total uterine length (mm) Mean |
91.3 |
85.3 |
||
| Uterine volume (cm |
34.6 |
20 |
||
| Uterocervical angle (degree) Mean |
139.7 |
125.3 |
||
Values are presented as Mean
Ultrasonographic evaluation of the 67 patients with IUD displacement revealed that 64 (95.5%) had a displacement, one (1.5%) had a perforation, and two (3%) had IUD displacement and pregnancy. Of these 67 patients, the presentations for IUD displacement were: low but not extending to the cervix (62.7%), low and extending to the cervix (19.4%), cervical (14.9%), and complete expulsion (3%).
Patient age and all the variables identified in univariate analysis as being
associated with IUD displacement with a p-value of
| Variable | Odds ratio | 95% CI | p-value | |
| BMI (kg/m |
1.27 | 0.93–1.74 | 0.126 | |
| Parity | 1.15 | 0.02–1.16 | 0.069 | |
| Vaginal bleeding (speculum examination) | ||||
| No | Ref | Ref | 0.038 | |
| Yes | 86.9 | 1.3–5885.3 | ||
| Cervical length | 0.53 | 0.25–1.12 | 0.097 | |
| Endometrial cavity length | 2.02 | 1.03–3.96 | 0.041 | |
| Total uterine length | 0.52 | 0.28–0.99 | 0.045 | |
| Uterine volume | 2.32 | 1.29–4.19 | 0.005 | |
| Uterocervical angle | 1.31 | 1.06–1.63 | 0.012 | |
BMI, Body mass index; CI, Confidence interval; IUD, Intrauterine device; Ref, Reference.
As shown in Fig. 4, ROC analysis revealed the UCA had significant predictive
value for IUD displacement (area under the curve (AUC): 0.865, 95% CI: 0.80–0.93, sample entropy (SE): 0.032,
p
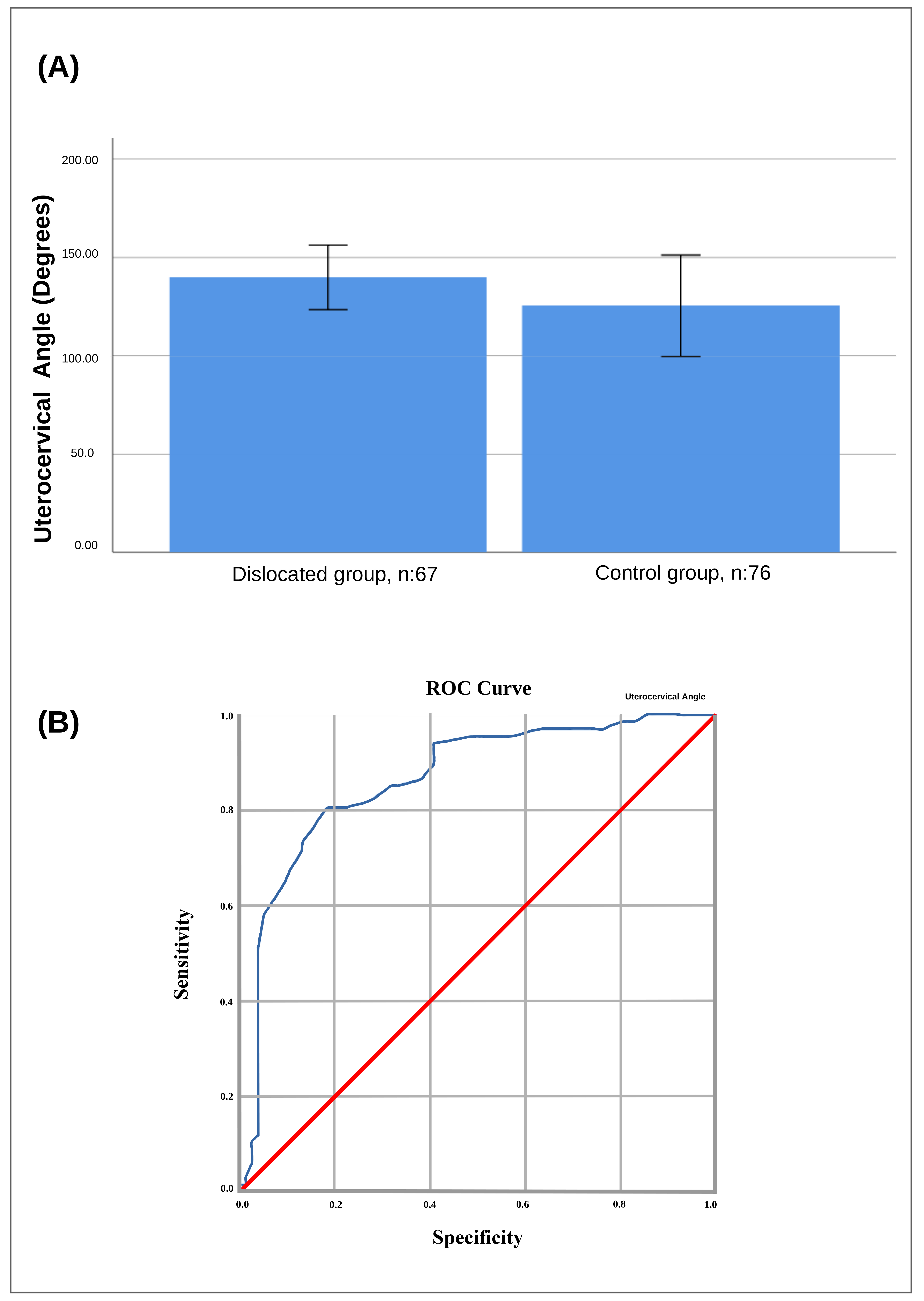 Fig. 4.
Fig. 4.Receiver operator characteristic curve and UCA degree averages
for patients who underwent copper IUD insertion. (A) The receiver operator
characteristic (ROC) area under the curve was 0.865 with a 95% confidence
interval of 0.80–0.93, standard error of the mean (SEM) of 0.032 (p
We performed a prospective cohort study to evaluate whether anterior UCA measurement was a predictor of IUD displacement. Our goal was to determine whether copper IUDs could be easily expelled by uterine contractions due to the flattened endometrial cavity and cervical line in the axial plane. The UCA was found to be significantly wider in women with displaced IUDs compared to those with a normal IUD position. Examination of secondary parameters revealed that endometrial cavity length, total uterine length, uterine volume, and vaginal bleeding were all positively correlated with IUD displacement.
Several previous studies have investigated the relationship between uterine
sonographic measurements and IUD displacement [5, 14, 15]. There is still no
consensus on whether the endometrial cavity length can impact IUD displacement.
No statistically significant correlation was found between endometrial cavity
length and IUD displacement [5, 6, 16, 17]. In contrast, a study by Castro
et al. [15] on 970 patients with Multiload (MLCu375) IUD found that
pregnancy rates were higher in women with an endometrial cavity length
Contradictory data has been published on the correlation between uterine volume
and the displacement of IUDs [14, 18, 19]. Although Moshesh et al. [19]
found no association between uterine volume and low-lying IUDs, their study was
limited by the small sample size. In contrast, another study reported a higher
discontinuation rate for levonorgestrel-releasing intrauterine devices (LNG-RIA)
in patients with adenomyosis and a larger uterine volume (
Abnormal vaginal bleeding has been consistently reported as the most frequent presenting symptom in patients with a displaced IUD [19, 20]. We found that women presenting with vaginal bleeding during examination had an 86.9-fold increased risk of IUD displacement. The reason for this very high risk is that pathologies causing abnormal bleeding were excluded before enrollment and the outpatient clinic administrations of patients outside of their standard period.
UCA can be used as an ultrasonographic parameter and also appears to be an
important anatomical factor in IUD displacement. Our results support the
hypothesis that as UCA gets wider, more IUD displacement occurs. Multivariate
logistic regression showed that a UCA
To our knowledge, the efficacy of UCA in predicting IUD displacement has yet to be reported in the literature. Major strengths of the present study include the comparison with several demographic and ultrasonographic variables, as well as the use of a single sonographer with a standardized protocol for the measurement of uterine dimensions and of all UCA measurements. Our study also has several limitations. First, the Coronavirus disease worldwide affected the number of patients attending their control visits which extended the time of the study. We tried to minimize this risk by using predetermined inclusion and exclusion criteria to screen the participants in our study. Secondly, we could not evaluate embedment as a type of displacement due to the absence of 3-D ultrasonography in our institution.
In conclusion, UCA measurement with ultrasonography before IUD insertion can be
used as a screening tool for predicting the displacement of copper IUDs. UCA can
be measured with a simple 2-D ultrasonography device on a standard mid-sagittal
transvaginal cervical image. Our results suggest that patients with a UCA
The datasets used and/or analyzed during the current study ara available from the corresponding author on reasonable request.
OK: Project development, Data Collection, Manuscript writing, Supervision; GNKK: Manuscript writing, Data collection; BY: Data collection, processed the images; IY: Data collection, Manuscript writing; AB: Made substantial contributions to conception and design, analyzed the data and interpreted data; IO: been involved in drafting the manuscript/reviewing it critically for important intellectual content, analyzed the data, final approval. All authors contributed to editorial changes in the manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work. All authors read and approved the final manuscript.
This study was approved by the Ethics Committee of the Health Sciences University, Istanbul Kanuni Sultan Suleyman Training and Research Hospital (approval number 2020-198). The study followed the ethics standards recommended by the Declaration of Helsinki. All patients gave written informed consent before enrollment.
Not applicable.
This research received no external funding.
The authors declare no conflict of interest.
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
