- Academic Editor
Background: This study aims to explore the risk factors inducing
bacterial vaginosis (BV) and establish a nomogram prediction model.
Methods: Single-factor analysis and multivariate logistic regression
were used to analyze the risk factors affecting the onset of BV. The selected
risk factors were incorporated into the R software to establish a nomogram
prediction model. The effectiveness of the proposed model was evaluated.
Results: The cleanliness of vaginal secretions above grade III accounted
for 90.86% (169/186) of the cases. Multivariate logistic regression analysis
showed that the use of nursing pads during non-menstrual periods, history of
miscarriage
Bacterial vaginosis (BV) is a common gynecological inflammation, which is associated with the decrease of the number of lactobacilli in vagina and the imbalance of flora caused by significant growth of Gardnerella vaginalis [1]. Previous reports have pointed out that about 60%–64% of BV patients are complicated with cervical erosion [2, 3]. The pathological features of BV are mucosal edema and inflammation, and the symptoms include abnormal leucorrhea, sexual pain and vaginal itching, which seriously affect the life of patients. Recent studies have found that BV is closely related to infertility, premature birth and abortion [4]. Women’s reproductive health is affected by multiple factors, such as biology, personal behavior, society, etc., which is difficult to be predicted clinically. Individualized prediction of BV risk and preventive intervention are helpful to reduce BV incidence and improve women’s living quality. However, there are few reports on individual prediction of BV. The nomogram, also known as Monograph, shows that [5], the nomogram prediction model has good discrimination and high degree of consistency in predicting adverse events. In this study, the clinical data of female patients undergoing physical examination in outpatient department were analyzed, the related risk factors affecting BV were discussed, and a nomogram model was established to predict the risk of BV individually.
In the experiment, a total of 883 women aged 26–62 years, with an average age
of (39.87
All participants in this study underwent vaginal examination by the same gynecologist. All included subjects had no history of vaginal irrigation within 24 hours, and underwent vaginal examination. Three cotton swabs were used to take the secretion of 1/3 section of vaginal wall for pH value detection, microscopic examination and amine test. Among them, one smear was added with normal saline to detect trichomonas, and one was sent to the laboratory for BV examination. BVBlue rapid detection method and Amsel gold standard method were used to detect polyamine. The other smear was heated, and then observed under a fixed mirror for clue cells.
According to the relevant standards of Obstetrics and Gynecology (9th Edition) [6]: ① increased vaginal secretion with thin character and fishy smell; ② positive amine test; ③ pH value of vaginal secretion above 4.5; ④ positive clue cells (prerequisite). BV was diagnosed when 3 of the above 4 items were positive.
A self-made questionnaire was used to investigate the information of patients, including age, education level, monthly income, abortion history, oral sex, sexual partner, whether to wash the vagina independently, sanitary pads used during menstruation, nursing pads used during non-menstruation, times of sexual activities per week, contraceptive methods, history of vaginitis, etc. All the patients agreed to participate voluntarily in the questionnaire survey. A total of 967 questionnaires were distributed, 883 of which were effectively recovered, with an effective recovery rate of 91.31%. The acquired data were checked and entered by two persons to ensure accuracy.
Data were processed by SPSS 22.0 software (IBM Corp., Armonk, NY, USA). Continuous variables conforming to
normal distribution are expressed in the form of mean
There were 186 cases of BV among 883 women undergoing gynecological examination,
and the incidence of BV was 21.06% (186/883). Among them, 17 cases were of grade
I–II, accounting for 9.14%; 169 cases were above grade III, accounting for
90.86%; 156 cases were positive in amine test, accounting for 83.87%. There
were 284 cases (32.16%) under 35 years old, 424 cases (48.02%) between 35 and
50 years old, and 175 cases (19.82%) over 50 years old. There were 346 cases
with educational background of junior high school and below (39.18%), 305 cases
(34.54%) with educational background of high school/technical secondary school,
and 232 cases (26.27%) with educational background of junior college or above.
There were 138 cases (15.63%) with monthly income less than ¥1000 (US
According to the occurrence of BV, 883 patients were divided into infected group
(n = 186) and uninfected group (n = 697). Univariate analysis results showed that
use of nursing pads during non-menstrual period, abortion history, oral sex,
self-vaginal irrigation, frequency of sexual activity per week and contraceptive
methods were the main factors affecting the occurrence of BV (p
| Clinical data | Total | Infected group (n = 186) | Non-infected group (n = 697) | p | ||
| Age (year) | 284 | 61 (32.80) | 223 (31.99) | 4.443 | 0.108 | |
| 35–50 | 424 | 98 (52.69) | 326 (46.77) | |||
| 175 | 27 (14.52) | 148 (21.23) | ||||
| Education degree | Junior high school and below | 346 | 86 (46.24) | 260 (37.30) | 5.139 | 0.077 |
| High school/technical secondary school | 305 | 59 (31.72) | 246 (35.29) | |||
| Junior college and above | 232 | 41 (22.04) | 191 (27.40) | |||
| Monthly income (¥ |
138 | 39 (20.97) | 99 (14.20) | 5.936 | 0.051 | |
| ¥1000–3000 (US $138.66–415.99) | 309 | 66 (35.48) | 243 (34.86) | |||
| 436 | 81 (43.55) | 355 (50.93) | ||||
| Marital status | Unmarried | 93 | 12 (6.45) | 81 (11.62) | 4.536 | 0.104 |
| Married | 618 | 139 (74.73) | 479 (68.72) | |||
| Divorced | 172 | 35 (18.82) | 137 (19.66) | |||
| Occupation | Farmer | 158 | 29 (15.59) | 129 (18.51) | 1.247 | 0.742 |
| Worker | 273 | 57 (30.65) | 216 (30.99) | |||
| Company employee | 280 | 64 (34.41) | 216 (30.99) | |||
| Other | 172 | 36 (19.35) | 136 (19.51) | |||
| Habit of wearing tights | None | 424 | 82 (44.09) | 342 (49.07) | 1.460 | 0.227 |
| Yes | 459 | 104 (55.91) | 355 (50.93) | |||
| Use of nursing pad during non-menstrual period | None | 651 | 110 (59.14) | 541 (77.62) | 25.881 | 0.000 |
| Yes | 232 | 76 (40.86) | 156 (22.38) | |||
| Abortion history (time) | 0 | 287 | 35 (18.82) | 252 (36.15) | 23.107 | 0.000 |
| 1 | 380 | 88 (47.31) | 292 (41.89) | |||
| 216 | 63 (33.87) | 153 (21.95) | ||||
| Oral sex | None | 778 | 154 (82.80) | 624 (89.53) | 6.349 | 0.012 |
| Yes | 105 | 32 (17.20) | 73 (10.47) | |||
| Sexual partner (each) | 0 | 82 | 11 (5.91) | 71 (10.19) | 5.625 | 0.060 |
| 1 | 692 | 145 (77.96) | 547 (78.48) | |||
| 109 | 30 (16.13) | 79 (11.33) | ||||
| Self-vaginal irrigation | None | 618 | 111 (59.68) | 507 (72.74) | 11.928 | 0.001 |
| Yes | 265 | 75 (40.32) | 190 (27.26) | |||
| Frequency of sexual activity per week (times) | 0–2 | 221 | 21 (11.29) | 200 (28.69) | 39.266 | 0.000 |
| 3–4 | 483 | 102 (54.84) | 381 (54.66) | |||
| 179 | 63 (33.87) | 116 (16.64) | ||||
| Contraceptive methods | Condom | 392 | 38 (20.43) | 354 (50.79) | 67.814 | 0.000 |
| Contraceptive | 164 | 42 (22.58) | 122 (17.50) | |||
| Intrauterine device | 233 | 65 (34.95) | 168 (24.10) | |||
| No contraception | 94 | 41 (22.04) | 53 (7.60) | |||
| History of vaginitis | None | 425 | 78 (41.94) | 347 (49.78) | 3.623 | 0.057 |
| Yes | 458 | 108 (58.06) | 350 (50.22) | |||
BV, Bacterial vaginosis.
Values were assigned to meaningful variables in single factor analysis, as shown in Table 2.
| Variable | Assignment |
| Use of nursing pad during non-menstrual period | None = 0, Yes = 1 |
| Abortion history | 0 = 0, 1 = 1, |
| Oral sex | None = 0, Yes = 1 |
| Self-vaginal irrigation | None = 0, Yes = 1 |
| Frequency of sexual activity per week | 0–2 = 0, 3–4 = 1, |
| Contraceptive methods | Condom = 0, contraceptive = 1, IUD = 2, no contraception = 3 |
IUD, Intrauterine device.
The significant variables of univariate analysis, including use of nursing pad
during non-menstrual period, abortion history, oral sex, self-vaginal irrigation,
frequency of sexual activity per week, contraceptive method, were taken as
independent variables (see Table 2), and the index of BV occurrence was taken as
a dependent variable. They were included in logistics regression equation for
multivariate analysis. The results showed that use of nursing pad during
non-menstrual period, abortion history
| Variable | SE | Wald ( |
p | OR | 95% CI | ||
| Lower limit | Upper limit | ||||||
| Use of nursing pad during non-menstrual period (1) | 0.435 | 0.190 | 5.250 | 0.022 | 1.545 | 1.065 | 2.241 |
| Abortion history | 18.624 | 0.000 | |||||
| Abortion history (1) | 0.459 | 0.219 | 4.407 | 0.036 | 1.583 | 1.031 | 2.431 |
| Abortion history (2) | 0.996 | 0.233 | 18.314 | 0.000 | 2.708 | 1.716 | 4.273 |
| Oral sex (1) | 0.417 | 0.255 | 2.683 | 0.101 | 1.517 | 0.921 | 2.499 |
| Self-vaginal irrigation (1) | 0.659 | 0.181 | 13.285 | 0.000 | 1.933 | 1.356 | 2.755 |
| frequency of sexual activity per week | 22.576 | 0.000 | |||||
| frequency of sexual activity per week (1) | 0.417 | 0.235 | 3.156 | 0.076 | 1.518 | 0.958 | 2.405 |
| frequency of sexual activity per week (2) | 1.166 | 0.261 | 20.009 | 0.000 | 3.210 | 1.926 | 5.351 |
| Contraceptive method | 15.016 | 0.002 | |||||
| Contraceptive method (1) | 0.408 | 0.242 | 2.854 | 0.091 | 1.504 | 0.937 | 2.415 |
| Contraceptive method (2) | 0.566 | 0.217 | 6.779 | 0.009 | 1.762 | 1.150 | 2.698 |
| Contraceptive method (3) | 0.982 | 0.272 | 12.996 | 0.000 | 2.670 | 1.565 | 4.553 |
| Constant | –3.076 | 0.301 | 104.464 | 0.000 | 0.046 | ||
BV, Bacterial vaginosis; OR, Odds ratio; CI, Confidence interval; SE, standard error; (1), Contraceptive; (2), Intrauterine device; (3), No contraception.
Based on the main influencing factors of BV obtained by multivariate logistic
regression model, a nomogram model was established by using R software (Fig. 1),
and the prediction probability associated with the sum of the index scores
represents the predictive value for BV occurrence risk. To be specific, 35 points
were assigned to the use of nursing pad during non-menstrual period, 39 points to
abortion history once, 85 points to sexual activity frequency
 Fig. 1.
Fig. 1.Nomogram model of bacterial vaginosis (BV) incidence.
According to the prediction model formula, the risk prediction value of BV was calculated. The area under the ROC curve was used to evaluate the nomogram. The area under the curve was calculated to be 0.789 (95% confidence interval (CI): 0.751–0.827, Fig. 2A) in this work, indicating that the nomogram had good discrimination. The calibration curve of nomogram was plotted, and the slope of calibration curve was close to 1 (Fig. 2B). Hosmer-Lemeshow goodness-of-fit test showed = 6.408 and p = 0.602, indicating that the nomogram model had high degree of consistency in predicting BV infection risk. The decision curve analysis (DCA) curve shows that the nomogram model can make valuable judgments and has good clinical applicability (Fig. 2C).
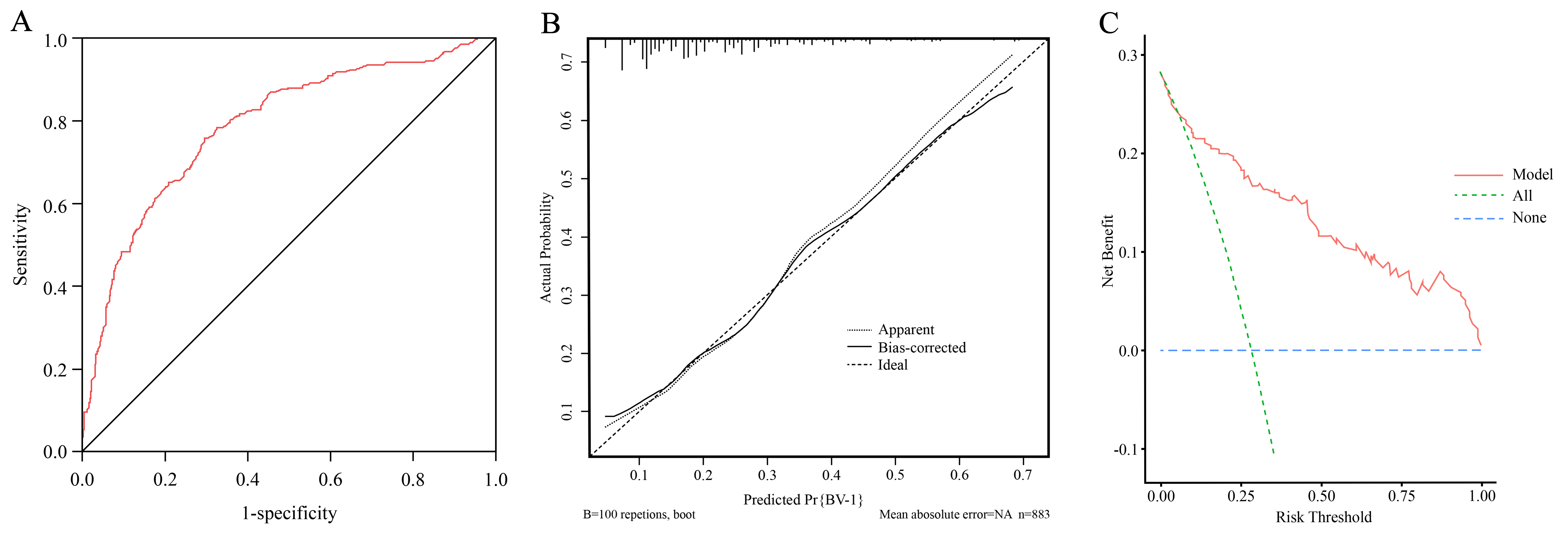 Fig. 2.
Fig. 2.Verification of nomogram model. (A) ROC curve analysis of nomogram model for predicting BV risk. (B) Calibration curve of nomogram model. (C) DCA curve of BV infection risk nomogram prediction model. ROC, receiver operating characteristic; BV, bacterial vaginosis; DCA, decision curve analysis
Vaginitis mostly occurs in women at childbearing age, with bacteria, trichomonas and candida as the main pathogens. Previous reports have pointed out that the incidence of BV is between 10% and 40%, and most women do not see a doctor because their symptoms are not obvious or there are no significant impact on their lives [7, 8]. In this study, the present situation of BV was investigated. The incidence of BV was 21.06% in 883 women who had physical examination in gynecological outpatient department of our hospital, which was higher than the value of 5.3% reported by Li M et al. [9], which may be related to the difference in sample size. The vaginal flora of healthy women is mainly Lactobacillus, and the lactic acid secreted by it can effectively maintain the acidic environment of vagina. The normal flora in vagina are mutually restricted and dependent, thus maintaining the microecological balance in vagina. Studies have shown that the occurrence of BV is related to the destruction of microecological balance in vagina [10]. 30–40 years old is the age with high incidence of vaginitis. BV can cause cervicitis and pelvic inflammatory disease. If the patient is pregnant, adverse perinatal outcomes may be resulted [11, 12]. In addition, recur easily recur and interfere with women’s daily life, so attention should be paid in clinical practices. At present, clinical scholars have attached great importance to women’s BV, and have conducted research on nursing and cross-sectional investigation [13]. However, how to realize individual prediction of BV is a clinical problem to be solved.
In this study, a nomogram prediction model was established based on the influencing factors of BV, such as use of nursing pad during non-menstrual periods, abortion history, frequency of sexual activity per week and contraceptive methods. The nomogram prediction model visually illustrates the contribution of the aforementioned factors to BV through a scoring system. Based on the sum of scores from these factors, each woman can be associated with a corresponding prediction probability. The nomogram showed that using nursing pad during non-menstrual period could increase the influence weight by 35 points, and self-vaginal irrigation could increase the influence weight by 55 points. At present, it is generally believed that personal hygiene habits and living habits are important factors affecting the occurrence of BV [14]. Vagina itself has self-cleaning and defensive functions, and the number of lactic acid bacteria is stable under acid-base equilibrium. Some women may experience increased vaginal discharge as a result of sexual activity, vaginitis, or other factors. To maintain hygiene, they may often use nursing pads. However, the use of nursing pads and self-vaginal irrigation during non-menstrual period can destroy the natural defense mechanism of vagina, change the restrictive relationship between microorganisms in vagina, lead to pathogen invasion, and affect the microecological balance in vagina, thus causing BV. It is suggested to strengthen public health education, improve women’s awareness of health care, correctly carry out vaginal cleaning, and use pads reasonably.
The nomogram proposed in this study shows that higher frequency of sexual activity per week can cause greater influence weight on BV. Previous studies have shown that the stability of vaginal lactobacilli is affected by sexual activity [15]. The reason may be that sexual activity can destroy the acidic environment in vagina, increase the pH value in vagina, and reduce the number of lactobacillus settlement. Scholars at home and abroad believe that contraceptive methods have an important impact on BV, and condoms are the protective factors of BV infection [16]. According to the nomogram of this study, the scores of influence weight of contraceptive pill, IUD and non-contraception were higher than those of condom contraception. It is suggested that condom contraception can block the pathogenic bacteria and reduce the risk of BV, which is consistent with previous reports [17]. Therefore, we should pay more attention to women’s sexual habits, especially the use of condoms, which not only helps to prevent BV, but also facilates the prevention of the spread of other sexually transmitted diseases. Abortion can damage endometrium, induce chronic inflammation, and destroy the normal defense mechanism of vagina. At the same time, abortion can also reduce immunity. This study shown that the risk of BV in women with more than 2 times of abortions was significantly increased. However, studies have also pointed out that BV has nothing to do with pregnancy outcomes such as premature delivery and miscarriage [18]. The relationship between induced abortion and BV needs to be further analyzed by a large-sample multi-center study.
To sum up, the proposed nomogram prediction model based on BV risk factors has good discrimination and high degree of consistency, which is helpful for medical staff to screen out the high-risk population of BV according to relevant data of physical examination women.
The datasets used during the present study are available from the corresponding author upon reasonable request.
XC—Manuscript writing, Project development, Data Collection; NL—Revised the paper, Data analysis, Data collection; HL and JL—Data collection. All authors contributed to editorial changes in the manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work. All authors read and approved the final manuscript.
This retrospective study involving human participants was in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by our institution’s ethics review board (approval number: 2021-C-113). All subjects gave their informed consent for inclusion before they participated in the study.
Not applicable.
This research received no external funding.
The authors declare no conflict of interest.
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
