1 1st Department of Otolaryngology - Head & Neck Surgery, Medical School, National & Kapodistrian University of Athens (NKUA), Hippokrateio Hospital, 11527 Athens, Greece
2 ENT Department, ELPIS General Hospital, 11528 Athens, Greece
3 Izmir Biomedicine and Genome Center (IBG), 35340 Balcova, Izmir, Turkey
4 Izmir International Biomedicine and Genome Institute, Dokuz Eylül University, 35340 Balcova, Izmir, Turkey
5 Department of Molecular Biology and Genetics, Faculty of Science, Muğla Sıtkı Koçman University, 48000 Kötekli, Muğla, Turkey
6 DNA Damage Laboratory, Department of Physics, School of Applied Mathematical and Physical Sciences, National Technical University of Athens (NTUA), 15780 Athens, Greece
† These authors contributed equally.
Abstract
Introduction: Several studies suggest that there is an association between the metastatic nodal tumor volume and the clinical outcome in patients with solid cancers. However, despite the prognostic potential of nodal volume, a standardized method for estimating the nodal volumetric parameters is lacking. Herein, we conducted a systematic review of the published scientific literature towards investigating the prognostic value of nodal volume in the carcinomas of head and neck, taking into consideration the primary tumor site and the human papillomavirus (HPV) status. Methodological issues: For this purpose, the biomedical literature database PubMed/MEDLINE was searched for studies relevant to the relationship of nodal volume to the treatment outcome and survival in head and neck squamous cell carcinoma (HNSCC) patients. Collectively, based on stringent inclusion/exclusion criteria, 23 eligible studies were included in the present systematic review. Results: On the basis of our findings, nodal volume is suggested to be strongly associated with clinical outcomes in HNSCC patients. Of particular note, there is an indication that nodal volume is an independent factor for further risk stratification for recurrence-free survival in patients with squamous cell carcinoma of the pharynx (oropharynx and hypopharynx). Extranodal extension (ENE) and HPV status should be also taken into consideration in further studies.
Keywords
- Head and neck cancers
- Nodal tumor volume
- Clinical outcomes
- Prognosis
- Systematic review
Accumulating evidence suggests that the presence of metastatic lymph nodes represents the most accurate predictor of clinical outcome for patients with head and neck squamous cell carcinoma (HNSCC) [1, 2]. Furthermore, human papillomavirus (HPV) infection (primarily type 16) is considered to be a prominent risk factor and an important prognostic indicator for HNSCC patients. Hence, HNSCC can be classified into two distinct types, HPV-positive and HPV-negative, with distinct mutational landscape, response to clinical treatment, and survival outcomes [2]. In a study by Gillison et al. (2012) [3], conducted in the United States, it has been demonstrated that there is a shift in the primary site distribution of HNSCC, with a steady increase of oropharyngeal squamous cell carcinoma (OPSCC) and a decline in cancers of the larynx and hypopharynx. This change is consistent with a decrease in tobacco use and the exposure to high-risk oncogenic HPV [3, 4]. Notably, there are distinct patterns of geographic variation in HPV-related oropharyngeal cancer, with higher prevalence in Western Europe; there are limited recent data available for Eastern Europe, Asia or Africa [5].
The prognostic value of the nodal tumor parameters including the extranodal extension (ENE) or extracapsular spread (ECS), the lymph node ratio (LNR) and the number of positive nodes (pN) in HNSCC, has been thoroughly investigated through systematic reviews and large-scale studies [6, 7, 8, 9]. ECS was found to have a negative effect on HPV-negative OPSCC and is recognized as a major criterion for the selection of high-risk HNSCC patients undergoing adjuvant chemotherapy in post-operative settings [7]. Moreover a combination of the ECS status and LNR value was found to have improved prediction power of outcomes in HPV-negative HNSCC patients [6]. The volume of the metastatic lymph nodes is another parameter that is considered to be of prognostic importance, given that a nearly linear relationship between the clonogenic tumor cell number and tumor control has been observed [10]. As far as the gross tumor volume (i.e., primary and nodal tumor volume) is concerned, there is a growing number of studies supporting its strong association with clinical outcomes and recurrence in HNSCC patients. Moreover, several studies suggest that tumor volume is the most important predictor of head and neck cancers, even superior to the Tumor, Nodes, Metastasis (TNM) staging [11, 12]. Of particular importance, in spite of the prognostic capacity of nodal volume, there is not currently a consensus regarding the measurement of nodal volumetric parameters, as highlighted by Lodder et al. [13].
The American Joint Committee on Cancer (AJCC) classification offers a reliable method for differentiating HNSCC patients with different prognoses. To date, TNM represents a staging system mainly focused on operability. TNM considers, in its prognostic stratification, only two-dimensional lymph nodes’ measurements or not at all, lacking quantitative volumetric evaluation of the tumor load. However, volumetric parameters are of great importance especially in the modern radiation therapy era where they could be useful in improving the accuracy of decision making in precision radiotherapy, than the simple measurement of the maximal diameter of regional lymph nodes. In the eighth TNM/AJCC edition several changes were introduced regarding the TNM staging classification for head and neck cancers. These changes are associated primarily with technical advances in diagnosis and treatment, as well as evolving knowledge regarding the prognosis and risk stratification of head and neck cancer patients from research and observational studies (e.g., inclusion of depth of invasion as a predictor for OSCC, inclusion of ENE for all non-viral head and neck cancers etc.) [14, 15]. Nonetheless, despite the significant advancements in diagnostic and therapeutic strategies that have taken place over the last years, the prognosis of HNSCC remains largely unfavorable, with a cumulative 5-year overall survival (OS) rate of 45–55% in patients with locally advanced HNSCC [16]. Therefore, research should be directed toward the identification of robust prognostic factors for the risk stratification of HNSCC patients.
Herein, we performed a comprehensive and updated systematic review of the literature on the prognostic value of nodal volumetric parameters, with respect to different primary sites, for HNSCC.
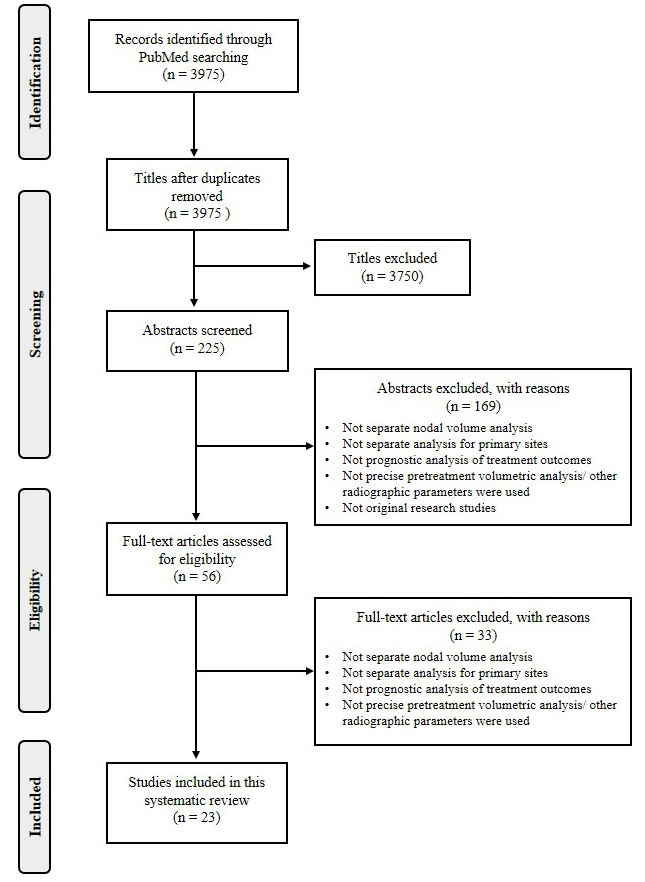
This systematic review was performed by following the PRISMA (preferred reporting items for systematic reviews and meta-analyses) statement [17] (Fig. 1). The bibliographic database PubMed/MEDLINE [18] was searched manually for relevant published studies reporting the association between nodal tumor volumes and prognosis in head and neck cancers, using the keywords: (((((((((((volum*) OR “Lymph Nodes/diagnostic imaging” [Mesh])) AND ((((“Head and Neck Neoplasms” [Mesh]) OR “Squamous Cell Carcinoma of Head and Neck” [Mesh])) OR hypopharyngeal))) NOT esopha*) NOT thyroid) NOT parathyroid) NOT sinonasal) NOT melanoma) NOT gland) NOT nasopharyn*. Regarding the primary tumor site, studies on neoplasms of the nasopharynx were not included in this systematic review, as they constitute a distinct epithelial malignancy entity with different etiology, pathogenesis and progression. Sinonasal squamous-cell carcinomas were not included as well, as their etiology, epidemiology, clinical features, and genetic profiles are quite distinct from those of the main head and neck cancer localizations, such as larynx, pharynx, and oral cavity cancers. The eligibility criteria for including studies in the present review were the following: (i) studies reporting the association between clinical outcomes and the nodal volume (not the total tumor volume), (ii) studies including separate analyses for each primary tumor site so as to minimize any confounding factors, and because of the diverge tumor imaging and volume measuring methods used across studies.
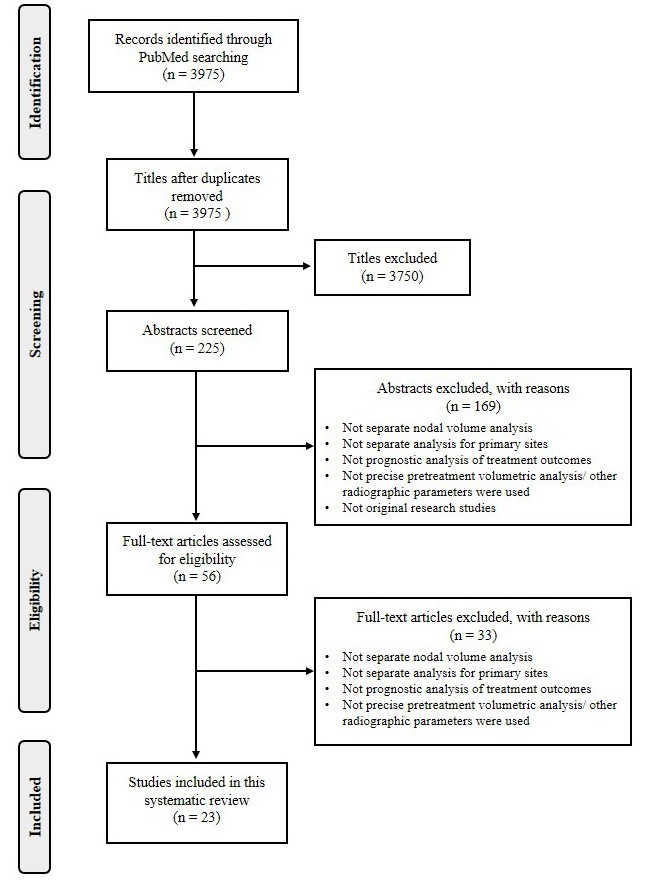 Fig. 1.
Fig. 1.PRISMA process flow diagram for study selection.
Studies were excluded from this review based on the following exclusion criteria: (i) no separate analyses for primary sites and nodal volumes were performed, (ii) no precise pretreatment volumetric analysis, and/or where other radiographic parameters were used, (iii) reviews, case reports, editorials, commentaries.
The quality of the retrieved studies was assessed independently by two authors (PTM. and AP). Any disagreement between PTM. and AP was resolved by a third investigator (EK). Respective data were extracted from the eligible studies and recorded into an ad hoc Excel worksheet.
Collectively, 3975 relevant records were retrieved from PubMed (up to 6 February 2021). After initial screening, 3750 titles and 169 abstracts were excluded because they were irrelevant to our study. A total of 56 full-text articles were assessed for eligibility. By applying strict inclusion and exclusion criteria, 23 studies were included in this systematic review (Fig. 1). The basic characteristics of the included studies are summarized in Table 1 (Ref. [19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41]), where the following information was recorded: first author’s surname and year of publication; primary tumor site; cancer stage; imaging method for tumor detection; type of tumor volume; type of therapy administered to patients; total number of patients; follow-up period; volumetric groups of patients; clinical treatment outcome; survival analysis statistic (e.g., hazard ratio) and the corresponding 95% confidence interval (CI) for the clinical outcome.
| First author, year | Primary site; cancer stage | Imaging technique; volume type | Type of treatment | Number of patients (N); | Volumetric groups | Treatment outcome; Survival statistic (95% CI), p value | |
| Follow-up period | |||||||
| Martens, 2021 [19] | Oropharyngeal, hypopharyngeal | PET-CT, DCE MRI; | curative (chemo) radiotherapy | N = 70 (Oropharyngeal = 56, hypopharyngeal = 14); | mean nodal volume in DCE MRI |
no significant differences in PET-CT volumetry | |
| DCEGTV (cm |
LRFS | ||||||
| Stages I–IV, with HPV status | Mean 22.1 months (interquartile range 14.3–29.4) | no proposed volumetric group | OS | HR = 1.18 (1.03–1.36), p = 0.018 | |||
| HPV-negative group (n = 44 patients) | HR = 1.20 (1.0–1.4), p = 0.027 | ||||||
| Fujii, 2019 [20] | Laryngeal, hypopharyngeal; | PET-CT; | Total laryngectomy and neck dissection | N = 88 (Hypopharyngeal = 61); | High risk Nmtv |
OS | |
| nMTV (SUV |
HR = 8.2 (2.5–31.9), p = 0.0004 | ||||||
| Stages III/IV | Intermediate risk ENE (+), Nmtv |
HR = 4.4 (1.4–16.7), p = 0.01 | |||||
| Low risk ENE (−), Nmtv |
Reference group | ||||||
| Safi, 2018 [21] | OCSSC; | CT; NV | Comprehensive neck dissection (level I to V), and postoperative radiotherapy | N = 100; | NV |
LR | |
| Stages III/IV (T4b excluded) | for locally advanced disease | HR = 20.926 (4.824–90.774), p | |||||
| Okazaki, 2018 [22] | Hypopharyngeal; | PET-CT; | Definitive RT ( |
N = 61; | In the subgroup of MTV-T |
OS | DSS |
| Stages III/IV | nMTV (SUV |
Median 21.7 (2.2–103.3) months | HR = 1.01 (1.00–1.03), p = 0.014 | HR = 1.02 (1.00–1.03), p = 0.012 | |||
| Cut-off value of nMTV = 73.5 mL | |||||||
| Dua, 2018 [23] | Pharyngeal (OPC, hypopharyngeal), no HPV status; | CT; TNV | Definitive concurrent chemoradiotherapy | N = 87 (OPC = 57); | OPC, TNV |
RC | |
| Stages III/IV | Median 18 (6–33) months | AUC = 0.974 (0.939–1.000), p = 0.001 | |||||
| Carpén, 2018 [24] | OPC, with HPV status; | CT; nGTV | Definitive chemoradiotherapy or IMRT | N = 91, p16 (+) = 72; | p16 (+) (nGTV as a continuous variable) | DDFS | LRC |
| HR = 1.02 (1.01–1.03), p = 0.005 | HR = 1.03 (1.01–1.05), p = 0.007 | ||||||
| Stages I–IV | p16 (+) Ngtv |
HR = 9.86 (1.05–93.03), p = 0.046 | ns | ||||
| p16 (+/−) (nGTV as a continuous variable) | HR = 1.02 (1.00–1.04), p = 0.022 | HR = 1.02 (1.00–1.04), p = 0.017 | |||||
| no differences found when nGTV was dichotomized by its mean value | |||||||
| Zhang, 2016 [25] | OCSSC; | PET-CT; | Surgery with or without radiotherapy or chemoradiotherapy | N = 122; | na | DFS | |
| Stages I–IV | nMTV (SUV |
Mean 2.4 (1.3–5.2) year | ns | ||||
| Kim, 2016 [26] | HPV-positive OPC; | PET-CT; | Surgery +/− radiotherapy or chemoradiotherapy | N = 86; | In high-risk patients (n = 54) with nMTV |
DFS | LR |
| Stages II–IV | nMTV(SUVmax |
Median 47.9 (5.1–102.6) months | HR = 1.09 (1.03–1.16), p = 0.004 | ||||
| p = 0.007 | ns | ||||||
| Davis, 2016 [27] | HPV-positive OPC; | CT; nGTV | Definitive chemotherapy and IMRT | N = 53; | na | DFS | |
| Stages III/IV | Mean 29 | HR = 1.021 (1.008–1.035), p = 0.001 | |||||
| (4–76) months | (not clear if multivariate analysis was performed) | ||||||
| Lin, 2015 [28] | Pharyngeal (OPC and hypopharyngeal), no HPV status; | CT, PET-CT; | IMRT +/− concurrent chemotherapy | N = 91, OPC = 49; | na | NRFS | DFS |
| Stages III/IV | nGTV, nMTV (SUV |
Median18 (6–69) months | ns | ns | |||
| Kendi, 2015 [29] | OCSSC; | PET-CT; | Surgery +/− radiotherapy or chemoradiotherapy | N = 36; | na | LRFS | |
| Stages I–IV | nMTV | Median 24.1 (8–44.5) months | ns | ||||
| Vainshtein, 2014 [30] | OPC with HPV status; | CT, PET-CT; | IMRT with concurrent chemotherapy +/− adjuvant neck dissection | N = 198, HPV (+) = 184 | na | LRF | |
| Stage III/IV | nGTV | ns (significant only in univariate analysis) | |||||
| Ng, 2014 [31] | Pharyngeal (OPC and hypopharyngeal), no HPV status; | CT, PET-CT; | IMRT with concurrent chemotherapy | N = 69 (OPC = 37); | na | 3-year neck control | |
| Stages III/IV | nGTV, nMTV (SUV |
ns (significant only in univariate analysis) | |||||
| Kikuchi, 2014 [32] | OPC with HPV status; | PET-CT; nMTV | Surgery +/− radiotherapy or chemoradiotherapy or radiotherapy +/− chemotherapy | N = 47 p16 (+) = 29; | Nmtv |
DFS | DSS |
| Stages I–IV | Median 30 (3–89) months | ns | HR = 5.0 (na), p = 0.04 | ||||
| Janssen, 2014 [33] | Laryngeal; | CT; nGTV | chemoradiotherapy | N = 270; | na | RC | |
| Stages II–IV | Median 44 (2–84) months | ns | |||||
| Alluri, 2014 [34] | HPV-positive OPC; | PET-CT; nMTV | Concurrent chemoradiotherapy or surgery or combination of both | N = 70; | na | EFS | |
| Stages III/IV | Median 25 (3–97) months | No multivariate analysis | |||||
| (significant only in univariate analysis) | |||||||
| Lok, 2012 [35] | OPC, no HPV status; | CT; nGTV | IMRT +/− concurrent chemotherapy | Ν = 340; | na | RC | |
| Stages I–IV | Median 34 (5–67) months | ns | |||||
| Chen, 2009 [36] | Hypopharyngeal; | CT; nGTV | Radiotherapy plus concurrent chemotherapy | N = 76; | na | NRFS | |
| Stages III/IVA | Median 37 (13–95) months | ns | |||||
| Tsou, 2006 [37] | Hypopharyngeal; | CT; nGTV | Radiotherapy plus concurrent chemotherapy | N = 51; | na | LC | |
| Stages III/IV | Mean 24.55 (5–76) months | significant only in univariate analysis | |||||
| Chao, 2004 [38] | OPC, no HPV status; | CT; nGTV | Definitive IMRT | N = 31; | na | DFS | LRC |
| Stages I–IV | Exp (B) = 1.06 (1.02–1.10), p = 0.05 | Exp (B) = 1.02 (1.00–1.04), p = 0.01 | |||||
| Hermans, 2001 [39] | Tonsillar, no HPV status; | CT; nGTV | Radiotherapy | N = 112; | Ngtv |
RC | |
| Stages I–IV | Mean 33 (2–121) months | significant only in univariate analysis | |||||
| Kawashima, 1999 [40] | Pharyngolaryngeal (oropharynx, pyriform sinus and supraglottic larynx), no HPV status; | CT; Nd | Definitive radiotherapy | N = 48; | Nd |
RC | Cause specific survival |
| Stages I–IV | p |
ns | |||||
| Jakobsen, 1998 [41] | Laryngeal, pharyngeal (no HPV status); | CT; Volumes of tumor burden of lymph node metastases | Radiotherapy | N = 280, Larynx = 71, Pharynx = 209 | NV |
DSS | |
| Stages I–IV | (except in 10 patients with laryngeal carcinoma who were subjected to surgery) | significant only in univariate analysis for each subsite | |||||
| Abbreviations: AUC, area under the ROC curve; CT, computed tomography; DCE, dynamic contrast-enhanced; DFS, disease-free survival; DSS, disease-specific survival; EFS, event-free survival; Exp (B), exponentiation of the B coefficient; HR, Hazard ratio; IMRT, intensity-modulated radiation therapy; LC, local control; LR, locoregional recurrence; LRC, locoregional control; LRF, locoregional failure; LRFS, locoregional recurrence-free survival; MTV-T, metabolic tumor volume of primary tumor; Nd, diameter of a sphere of which the volume is equal to the sum of volumes of the metastatic adenopathies; nGTV, nodal gross tumor volume; nMTV, nodal metabolic tumor volume; NRFS, nodal relapse-free survival; NV, nodal volume; OCSCC, oral cavity squamous cell carcinoma; OPC, oropharyngeal carcinoma; OS, overall survival; PC, pharyngeal carcinoma; PET-CT, positron emission tomography-CT; RC, regional control; SUV, standardized uptake value; TNV, total nodal volume. *na: not available data; ns: not significant in univariate analysis. | |||||||
The majority of the studies included in this review focused on squamous cell
carcinomas of the pharynx (oropharynx, hypopharynx or both) (Table 1, Ref. [19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41]; Table 2, Ref.
[19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 41]). In all of those, nodal tumor volumetry was assessed using
pre-treatment imaging (CT, PET-CT, MRI). In most of the studies, the volume of
the primary tumor and the involved metastatic lymph nodes were automatically
measured using a radiotherapy treatment planning software, within a region of
interest contoured at workstation software, preferably by two readers (i.e.,
radiologist or nuclear medicine physician or head and neck radiation oncologist
or otolaryngologist). None of the studies included information about the
volumetric parameters for the surgical specimen. In addition, among the MRI
studies screened for eligibility, only two studies had conducted concise
volumetric analysis. However, only one MRI study [19] was included in this
review, while the other study failed to meet the inclusion criteria, as nodal
volumes were studied separately for ipsilateral and contralateral nodes [42]. In
the volumetric analyses where CT was used, nodal gross tumor volume (nGTV) was
the most frequently used term to describe the cumulative metastatic lymph node
volume. In those studies where the PET-CT parameters were analyzed, we presented
results related only to nodal metastatic tumor volume (nMTV) and not the total
lesion glycolysis (TLG), or the mean or maximum standard uptake value
(SUV
| Primary tumor site | Number of related studies | Total number of patients in all related studies | High-risk patient volumetric subgroups proposed by study | Significantly affected treatment outcome | |
|---|---|---|---|---|---|
| Oropharynx | 13 studies [19, 23, 24, 26, 27, 28, 30, 31, 32, 34, 35, 38, 39] | HPV (+) | nGTV |
LRFS [19], RC [23], LRC [38], DFS [26, 27, 28], DSS [32] | |
| 1227 | 518 | nMTV |
|||
| HPV (−) | |||||
| 83 | |||||
| No HPV status | TNV |
||||
| 626 | |||||
| Hypopharynx | 8 studies [19, 20, 22, 23, 28, 31, 36, 37] | 367 | Nmtv |
OS [20, 22], DSS [22] | |
| Nmtv |
|||||
| Larynx | 3 studies [20, 33, 41] | 368 | ns | ||
| Oral Cavity | 3 studies [21, 25, 29] | 258 | NV |
LR [21] | |
Most of the eligible studies on OPC were published after 2014 and included data associated with the HPV status (Table 1). Notably, in these studies, the vast majority of the OPC patients were HPV-positive. The results of HPV-positive OPC patients indicate a potentially significant prognostic value of the nodal volumetric parameters. However, there is a disagreement about the terminology used for end-points to define treatment failure and the level of significance for each end-point in the treatment outcomes. Disease-free survival (DFS) is the end-point mostly associated, with statistical significance, to nodal volume. In order to further our understanding on the prognosis of HPV-positive OPC patients, a meta-analysis would be useful, though this might be difficult due to the heterogeneity in the available studies. Conversely, there are limited data in the current literature supporting the potential use of nodal volume in the prognosis of HPV-negative patients with OPC. Nonetheless, in the most recent study selected for this review [19], which included patients with pharyngeal carcinomas, a separate analysis was also conducted for the HPV-negative group. Interestingly, nodal volume in dynamic contrast-enhanced (DCE) MRI was significantly associated with recurrence-free survival (RFS) in multivariate analysis.
Regarding hypopharynx alone, an association between nodal volume and treatment outcomes was found mainly in univariate and not in multivariate analyses; for oral cavity a significant association was observed only in the advanced stages (III and IV) of squamous cell carcinomas (Table 1).
None of the studies included in the present review used the 8th edition TNM/AJCC classification for staging head and neck cancer patients, whilst only one clearly included ENE in multivariate analysis [20]. In the same study, which included mostly patients with hypopharyngeal squamous cell carcinoma, it was demonstrated that there is a statistically significant risk for patients with large nodal tumor volumes, regardless the presence of ENE [20].
In some studies patients were stratified into high-risk volumetric subgroups
[20, 21, 23, 25, 44, 45]. The great majority of these studies (5 out of 6)
focused on carcinomas of the pharynx (two studies [20, 45] on hypopharyngeal SCC
and three studies [21, 23, 25] on oropharyngeal SCC). The proposed nodal volume
cutoffs appeared to vary slightly among the studies of the oropharynx (nGTV
In this systematic review, we focused predominantly on the detection of groups of patients (regarding both the primary tumor site and the HPV status) where the nodal tumor volume can be used as a prognostic imaging biomarker for HNSCC patients. Notwithstanding, articles screened for eligibility in this review, apart from the heterogeneous methods applied for volume measurements, they also had other limitations which did not allow us to assess the prognostic value of nodal volumetric parameters. Full-text articles reporting the total tumor volume (both primary plus nodal tumor volume) instead of the nodal volume separately were also screened in this review, while the majority of those contained all primary tumor sites with no separate analysis for each one of them. Another serious limitation of our study was the lack of multivariate analyses in many of the studies examined for eligibility. Notably, even two studies [42, 46] which include multivariate analysis regarding the prognostic significance of nodal volumes failed to meet our inclusion criteria. In particular, Ljumanovic et al. [42] conducted only separate analysis regarding ipsilateral and contralateral lymph node volume and Vergeer et al. [46] did not include a separate analysis of the primary tumor site.
In order to minimize the aforementioned limitations so as to avoid any confusion
and hasty conclusions, we considered as eligible only the articles where the
nodal tumor volume was separately analyzed for each primary tumor site. In those
articles, we investigated whether there is a statistically significant
(p value
The identification of volumetric groups of patients might have potential utility in clinical decision making for locally advanced head and neck cancers. Of note, in the case of treatment de-escalation for HPV-positive oropharyngeal cancers, the first results from De-ESCALaTE HPV, an open-label randomized controlled phase 3 trial [47], showed that compared to the standard cisplatin regimen, cetuximab had a significantly detrimental effect on tumor control, thereby leading to the suggestion that combinatorial therapy of cisplatin and radiation should be used as the standard of care for HPV-positive low-risk patients who are able to tolerate cisplatin. Low-risk patients were defined according to the Ang classification [48], that is, the patient-derived tumor cells had to be p16-positive on p16 immunohistochemistry, and the patients had to be non-smokers or have a self-reported lifetime cigarette history of less than 10 pack-years.
Moreover, volumetric stratification might be more appropriate for patients where different treatment modalities were used. The observed differences in the proposed volumetric subgroups concerning patients with carcinomas of the oropharynx and hypopharynx, indicate that in surgically treated patients with pharyngeal carcinomas, lower nodal volumetric cutoffs should be used for the risk stratification of those patients and more aggressive postoperative treatments might be proven beneficial. However, this has to be further investigated, separately for HPV (+) and HPV (–) cases, in large-scale studies.
In high-risk patients, immunotherapy could also be used in the adjuvant setting, even for newly diagnosed cases of metastatic nodal disease. Such therapeutic protocols are in line with recent data supporting the use of immunotherapy with checkpoint inhibitors, such as Nivolumab and Pembrolizumab, in recurrent and/or metastatic HNSCC [49].
Nodal volumetric analysis in patients with oropharyngeal, both HPV-positive and HPV-negative, and hypopharyngeal carcinomas appears to represent a challenging and promising field for research. Of particular note, in a quite recent systematic review [44], it was shown that the locoregional recurrence rates for HPV-negative (26%) patients are significantly higher (i.e., almost three times higher) as compared to HPV-positive (9%) OPSCC patients. This finding, in combination with the results of a multicentric study by Culie et al. (2021) [45], wherein primary surgical treatment in patients with p16-negative OPSCC was found to be associated with improved overall survival (OS), disease-specific survival (DSS) and RFS, further supporting that patients with p16-negative OPSCC represent a group at high risk for recurrence, and metastatic nodal tumor volume could serve as an independent and decisive factor for risk stratification. The need remains, though, for standardizing the measurement of nodal volume. Hitherto, volumetry is mainly assessed by CT and PET-CT, albeit in surgically treated patients. Tumor volumetric data can also be derived from the histopathological analysis of neck dissection surgical specimen. The development of deep learning neural network algorithms might also be useful for the risk stratification of patients regardless of the volumetric method used. Furthermore, the release of the new edition of TNM classification for head and neck cancers should be taken into consideration in future meta-analyses. In order to clarify whether and in which groups of patients the addition of nodal volume could improve the predictive capacity of the 8th edition of the TNM/AJCC, values of variables referring to the TNM classification should be updated accordingly, before conducting multivariate analysis.
In the present study, we have conducted a systematic review in order to assess further the prognostic potential of nodal tumor volume in the cancers of the head and neck, taking into consideration the lack of a standardized protocol for measuring the nodal volume. Based on our findings, nodal volume could be considered as a candidate imaging biomarker for monitoring and predicting diverse clinical outcomes in HNSCC patients. Future studies should focus on determining a standard methodology for assessing nodal volumetric parameters and their potential utility in the imaging, prognostication and treatment of head and head cancers. Moreover, further research is required, where both the ENE and the HPV status will be taken into consideration in patients with pharyngeal squamous cell carcinomas, in order to identify possible subgroups of patients with considerably higher risk for locoregional recurrence, who might benefit from different therapeutic and/or post -treatment follow-up approaches.
AGG and EK conceived the study; AGG, PTM and EK designed and supervised the study; PTM and AP analyzed the data; PTM, AP, RÜ, IM, AGG and EK wrote the manuscript; PTM, AP, RÜ, IM, AGG and EK revised the manuscript. All authors reviewed and approved of the final manuscript.
Not applicable.
Thanks to all the peer reviewers for their constructive comments and suggestions.
This study received no external funding.
The authors declare no conflict of interest.
HNSCC, head and neck squamous cell carcinoma; OPSCC, oropharyngeal squamous cell carcinoma; HPV, human papillomavirus; TNM, Tumor, Nodes, Metastasis; CT, computed tomography; PET-CT, positron emission tomography-CT; MRI, magnetic resonance imaging.