1 Health Neuroscience Collaboratory, College of Health Solutions, Arizona State University, Phoenix, AZ 85004, USA
2 Department of Psychiatry, University of California, San Diego, CA 92093, USA
Abstract
This Opinion piece discusses several key research questions in health neuroscience, a new interdisciplinary field that investigates how the brain and body interact to affect our health behavior such as health mindsets, decision-making, actions, and health outcomes across the lifespan. To achieve physical, mental, and cognitive health, and promote health behavior change, we propose that the prevention and treatment of diseases should target the root causes—the dysfunction and imbalance of brain-body biomarkers, through evidence-based body-mind interventions such as mindfulness meditation and Tai Chi, rather than dealing with each symptom or disorder in isolation through various treatment approaches.
Keywords
- health neuroscience
- integrative health
- behavior change
- brain-body interaction
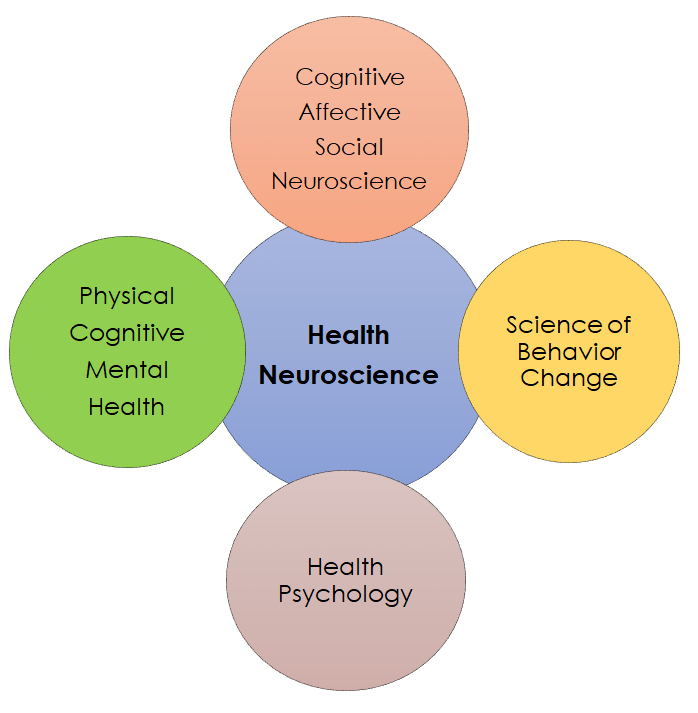
Health neuroscience was first proposed in 2014, a field that lies at the interface of health psychology and neuroscience and focuses on understanding the interplay between the brain and physical health over the lifespan [1]. In the 2020 Health Neuroscience Special Issue in Social Cognitive and Affective Neuroscience, the author proposed health neuroscience should integrate with social, cognitive, and affective neuroscience, and focus on the three goals—to understand the brain as a predictor, mechanism, and outcome [2]. Here we extend the framework of health neuroscience by adding the science of behavior change and integrative health (e.g., physical, mental, and cognitive health), and discuss several key research questions in health neuroscience, as well as potential applications to achieve integrative health and promote effective health behavior change.
As shown in Fig. 1, Health Neuroscience is a new interdisciplinary field encompassing research from (but not limited to) cognitive, affective, and social neuroscience, health psychology, physical, mental, and cognitive health, and the science of behavior change. Health behavior includes at least health mindsets, decision-making, and actions that contribute to health outcomes across the lifespan. Health behavior change is the process of adopting and maintaining healthy behaviors that contribute to overall well-being and prevent or manage health conditions. By adopting and maintaining health behaviors, individuals can not only prevent the onset of certain health conditions but also effectively manage existing health issues, leading to improved overall health and well-being. Therefore, health behavior change plays a crucial role in shaping health habits and outcomes. Health neuroscience focuses on understanding the relationship between the brain/mind, body (physiology), and overall health and well-being, and how the brain/mind and body work together to affect health behavior and outcomes [3, 4]. This Opinion piece discusses several key research questions in health neuroscience.
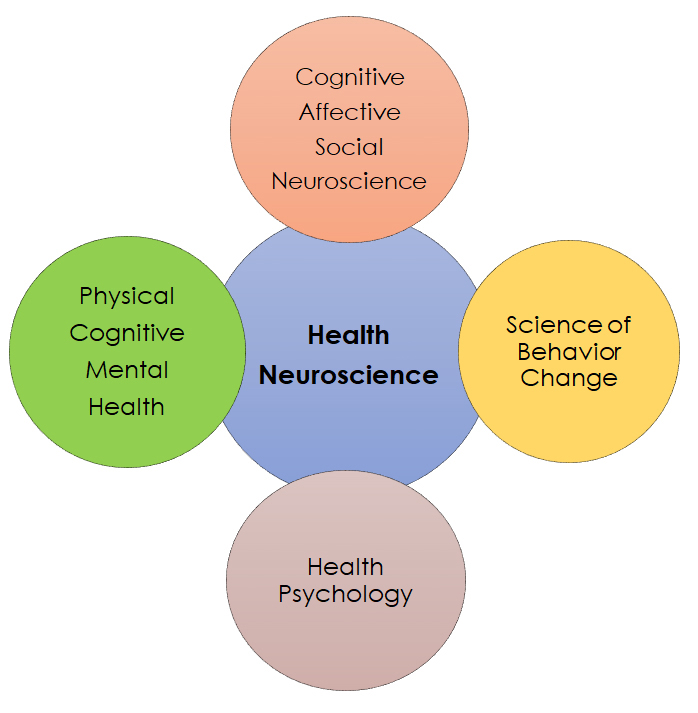 Fig. 1.
Fig. 1.The framework of health neuroscience.
Behavior change, in particular health behavior change, is one of the most important achievements in our lives. To maximize overall health, wellness, and longevity, people need evidence-based approaches to manage their health behaviors and change behavior effectively when needed. Although there are various health behavior models, behavior change involves dual processes—both automatic (implicit, unconscious) and controlled (explicit, conscious) [5, 6, 7, 8, 9]. Most behavior change models focus on the controlled (explicit) process consciously. A controlled process involves a conscious intention and motivation to change behavior [10]. For example, mindset change is a commonly used approach to consciously change behavior. A longitudinal study tracked USA adults for years by asking them two questions: (1) how much stress did you experience last year and (2) do you believe that stress is harmful to your health? Based on the public death records, the study examined who died or not during the study period. Interestingly, people who experienced a lot of stress last year had a 43% increased risk of dying. However, this was only true for the people who believed that stress is harmful to health, not for those who did not. These findings suggested that people died prematurely, not from stress, but from their beliefs (mindset on stress) that stress is bad and harmful [11]. Relatedly, other studies using nationally representative samples also indicated that perceptions about health behaviors (e.g., level of physical activity) play an important role in shaping health outcomes [12].
Compared to conscious behavior change, the mechanisms of unconscious behavior change remain largely unknown. Growing evidence has suggested that unconscious processes such as implicit cognition, implicit attitude, implicit emotion or affect, and implicit motivation can all influence health behavior [13, 14, 15]. However, how unconscious processes initiate and maintain behavior change and form habits remains poorly understood. One direction of future research is how to promote effective behavior change through unconscious processes and how to combine both conscious and unconscious behavior change for better health outcomes [3, 16]. So far, only a few studies have investigated the neural correlates underlying health behavior change. A recent article reviewed the latest findings of the conscious processes of health behavior change and concluded that initiation and maintenance of behavior change are based on motivation and reward mechanisms. Specifically, the medial prefrontal cortex (mPFC) and striatum are actively involved [3, 16]. Similarly, self-control networks such as the anterior cingulate cortex (ACC) and adjacent mPFC and striatum also play a crucial role in behavior change [3, 17, 18, 19, 20, 21, 22]. Therefore, unconscious behavior change may also recruit similar self-control networks, and motivation and reward networks [3]. Future research is warranted to understand the brain mechanisms of unconscious processes of behavior change.
Brain/mind and body are often treated as two separate identities. The brain/mind is largely considered to be the center of command, giving out instructions and guiding how the body functions in everyday life. However, the brain and body cannot be separated in a living system. For instance, the gut-brain axis is a demonstrated brain-body connection. Multiple pathways support the communication between gut and brain, including neurologic, immune, endocrine, and metabolic pathways. Through bidirectional communication and interaction, not only does the brain affect gut function, but the gut also affects brain function and structure. Moreover, the gut microbiota plays an important role in facilitating communication between the gut and brain, as well as in affecting behavior [23]. Differences in gut microbiome have been detected between healthy and patient populations. For example, the gut microbiome contributes to the pathogenesis of neurological disorders such as Alzheimer’s disease, and Parkinson’s disease [24]. While fecal samples in gut microbiome research have proven to be valuable, they also come with disadvantages. For example, fecal samples tend to have substantial variability in microbial composition even within the same individual over time. Factors such as diet, medications, and overall health can influence the microbiome. The microbial composition can also vary along the gastrointestinal tract and it may represent only a portion of the entire gastrointestinal tract. Moreover, fecal samples often provide a snapshot of the gut microbiome at a specific point in time and cannot capture real-time changes or dynamic changes in the microbial community [25, 26]. Therefore, these methodological challenges call for immediate solutions. To address these major research gaps in brain-body interaction research, there is a crucial need for advances in technology that could enable simultaneous and direct measures of both brain and body changes.
Similarly, the brain-heart connection is another prominent example. Research showed that heart-related genes can explain up to 14% of heritability in brain function and structure, suggesting a potential relationship between heart and brain health [27]. Relatedly, recent studies demonstrated that human aging involves the interaction between both the brain and multiple organs including cardiovascular, pulmonary, musculoskeletal, immune, renal, hepatic, and metabolic systems [28]. That is, body aging and brain aging are related to each other. Moreover, poor physical health across the body and organ systems is more pronounced in individuals with common psychiatric disorders such as anxiety, depression, bipolar disorder, and schizophrenia than in healthy individuals. Additionally, deterioration in physical health is more severe than deterioration in brain health for those with psychiatric disorders, suggesting that psychiatric disorders are unlikely to be diseases that only concern the brain and the mind [29]. Therefore, health and diseases that concern the brain are also linked to health and diseases that concern the body. Unfortunately, most of the treatment approaches to date have focused on treating psychiatric symptoms while neglecting co-occurring physical symptoms. However, current imaging technology measures the heart and brain separately and cannot track real-time brain-heart interaction and changes.
To date, there are many unanswered questions regarding how the brain and body interact to contribute to health and diseases across the lifespan. For example, does the relationship between brain and body vary across the lifespan? As humans, we go through various stages of development with significant body and brain changes, but they do not often occur at the same pace. Could they be more strongly associated with each other early in life but not later in life or vice versa? Relatedly, because of the close brain-body connection in psychiatric disorders, could treating physical illnesses in patients with psychiatric disorders ameliorate psychiatric symptoms? Currently, there has not been a lot of research into potential interventions that could improve both body and brain health. Could these approaches be implemented in healthcare settings to improve treatment efficacy and outcomes? Research has shown that body aging can accelerate brain aging and having an older age of one organ system can accelerate the aging of another organ system. Are there potential subtypes of organ aging? For instance, two organ systems may age together in some individuals, leading to specific behavioral and cognitive problems that are different from the behavioral and cognitive problems related to the aging of other organ systems. Or does aging across most organ systems contribute to overall poor cognitive, physical, and mental health? Investigating the brain-body connection during aging provides additional insights into whether the body and brain reciprocally influence and contribute to each other’s health across the lifespan. Moreover, such understanding will systematically advance our health promotion strategies and treatment approaches.
Conventional medicine is the mainstream medical practice and treatments that focus on disease treatment mainly using medications, therapies, and surgeries. It has made advancements in treating many disorders and specific symptoms but also has its limitations, for example, it does not always address the root causes of certain chronic diseases. In addition, medical spending has significantly increased, such that prescription drug spending has been the fastest-growing goods/service category in the USA to treat each symptom or disorder in isolation. Back in the 1950s, about 2–3% USA Gross Domestic Product (GDP) was used for health care/medical spending, whereas in the 2000s, it increased to almost 20% of GDP. However, the general public has not received better and higher quality health care [30]. Given that medications often have side effects, in some cases, conventional medicine has already incorporated certain aspects of complementary and alternative therapies, such as meditation, acupuncture, cognitive training, and art therapy [3, 22, 31], with a focus on treating the whole person rather than one organ or symptom to achieve better health outcomes.
The integrative health model has three components—self-care, complementary and alternative medicine, and conventional medicine. The self-care approach emphasizes that we should take an active role in maintaining our health through intentional practices and behaviors. It recognizes that we have the responsibility to act to promote physical, mental, emotional, cognitive, and social health (e.g., harmony with others). Self-care plays a crucial role in integrative health, as it affects the effectiveness of the other two components. For example, it can change our passive attitudes, mindsets, and actions in a positive and actionable way, rather than only waiting for physicians to fix our problems and give us health back through conventional care. Self-care requires a high level of self-control to continuously support health behavior change and desired health outcomes [3, 17, 32]. Self-care often includes behavior change and lifestyle approaches (e.g., nutrition, exercise) to promote wellness and emphasize our responsibilities, awareness, and care action [3, 32]. Therefore, there is an urgent need to apply integrative health approaches to prevent and treat diseases, not only to ameliorate symptoms but also to address the root causes of diseases through our efforts and actions.
The National Institutes of Health’s Research Domain Criteria (NIH’s RDoC) project is an example in response to the growing awareness of the diagnosis and treatment issues in conventional medicine [33]. In the past, mental disorders were diagnosed based on the number and type of symptoms. This approach has led to obvious benefits but also created problems with disease heterogeneity. For instance, two individuals can be diagnosed with the same disorder despite having few symptoms in common. Relatedly, mental disorders often involve comorbidities, as individuals may exhibit symptoms of depression and anxiety at the same time. Therefore, targeting the common brain-body dysfunction and imbalance may be a better approach, as such dysfunction and imbalance may be the precursor of symptoms and disorders. In contrast, targeting different symptoms through symptom relief/reduction to prevent and treat disorders could not directly address the root causes that give rise to these symptoms [3, 4, 19].
Growing evidence indicates that based on the integrative health model, it is possible to target the root causes—the dysfunction and imbalance of brain-body biomarkers through evidence-based integrative body-mind interventions. The human being is a complex living system that can self-regulate and self-organize to maintain balance, stability, and integrative health. This can be achieved through the active homeostatic process of adapting (also called allostasis) during changing conditions or challenges, such as from healthy to less healthy (symptoms), and to disease stages or vice versa [3, 17, 19, 34]. Through efficient self-control, our self-organized system can promote and restore health during the stages of the bidirectional health and disease continuum—from disease to less healthy (symptoms) to healthy. Research findings indicate strengthening self-control through the central nervous system (CNS, brain) and autonomic nervous system (ANS, body) interaction and optimization can help ameliorate different symptoms and treat disorders [3, 8, 17, 19, 20, 21, 22]. Moreover, evidence-based body-mind interventions have shown promise to effectively change brain-body biomarkers, improve self-control, and ameliorate brain-body dysfunction and imbalance—the precursor of symptoms and disorders [3, 19, 35, 36, 37].
As an illustrative example, we here describe integrative body-mind training (IBMT) to provide evidence on the positive effects of body-mind interventions on changing brain-body biomarkers, improving self-control, achieving integrative health, and accordingly, ameliorating symptoms, and treating disorders. Based on our randomized controlled trials (RCTs) [8, 17, 19, 20, 21, 22, 32, 35, 36], one of the key mechanisms by which IBMT induces positive effects on health is enhancing the interaction and optimization between brain/mind and body—a process that involves both the CNS and ANS. In an RCT using 5 consecutive sessions of IBMT vs. relaxation training (30 minutes per session for 5 days), participants practiced either IBMT or relaxation training while their brain activity in self-control networks was being recorded. Specifically, the midline anterior cingulate cortex (ACC) was recorded along with physiological indexes including respiratory rate and amplitude, heart rate, heart rate variability (HRV), and skin conductance response that assess the ANS function [35]. Results indicated positive physiological changes with the greater parasympathetic activity of the ANS and increased frontal midline ACC theta power following 5 sessions of IBMT than relaxation training. Moreover, midline ACC theta power correlated with high-frequency HRV (HF-HRV). Together, these findings indicate that the body (indexed by HF-HRV) and brain (indexed by midline ACC theta power) work together to support the brain and body functioning through strengthening self-control, and thus may regulate brain and body dysfunction and imbalance, ameliorate symptoms, and treat disorders [8, 17, 19, 20, 21, 22, 32, 35, 36]. Our further research applied IBMT in disorders such as addiction, anxiety, and depression, and showed that 5–20 consecutive sessions of IBMT (30 min per session) increased both functional and structural brain plasticity in self-control networks, particularly in the ACC and adjacent medial prefrontal cortex, posterior cingulate cortex, and striatum (brain biomarkers), as well as the parasympathetic activity of the ANS (body biomarkers). These brain changes were observed along with reductions in addiction (e.g., craving and substance use), emotion dysregulation, stress, and symptoms of anxiety and depression [3, 19, 35, 36]. Our findings also highlight that evidence-based body-mind interventions may be promising approaches for promoting the synergistic engagement of brain and body to achieve the desired behavior change and health outcomes.
However, some questions remain to be investigated. For example, what are health-relevant physiological responses predicted by or related to brain changes or vice versa? How to develop biomarkers for predicting differential responses to established treatments of mental disorders? How to better inform individual-level treatment selection (precision mental health) using biomarkers? Future research is needed to address these crucial gaps.
In this Opinion piece, we mainly focused on several research gaps in the field of health neuroscience. To achieve integrative health and promote health behavior changes, we proposed that the human being as a self-regulating and self-organizing system can maintain its rehabilitation, balance, and stability. Moreover, prevention and treatment of diseases should target the root causes—the dysfunction and imbalance of brain-body biomarkers rather than dealing with each symptom or disorder in isolation through various treatment approaches. We discussed the self-control network as a potential mechanism that supports integrative health following evidenced-based body-mind interventions. However, other systems such as the reward system also support motivation, self-control, and behavior change that are closely linked to health and well-being [3, 8, 19, 20, 21, 22, 36]. Future work is needed to explore the interaction between self-control and reward systems that improve and optimize behavior change and health outcomes. We also discussed how body-mind interventions can improve neuroplasticity and support health outcomes. Further investigation is warranted to understand how to target promising body-brain biomarkers early in life to optimize behavior change and health outcomes. We acknowledge that given the scope of the Opinion piece, we selectively reviewed only a manageable subsample of possible studies related to health neuroscience approaches and that there are other exciting new research directions and findings that incorporate neuroscience, physiology, and behavioral science to investigate different topics of health neuroscience. We hope that this Opinion piece will encourage further research and technology advances to improve our understanding on human health across the lifespan.
YYT conceptualized and designed the study. YYT and RT wrote the manuscript. YYT and RT designed the figures. YYT and RT reviewed the manuscript. Both authors contributed to editorial changes in the manuscript. Both authors read and approved the final manuscript. Both authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
Not applicable.
Not applicable.
This work was in part supported by the National Institutes of Health (grant R33 AT010138).
The authors declare no conflict of interest. YiYuan Tang is serving as one of the Editorial Board members of this journal. We declare that YiYuan Tang had no involvement in the peer review of this article and has no access to information regarding its peer review. Full responsibility for the editorial process for this article was delegated to Gernot Riedel.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.