1 Department of Cardiology, Affiliated Hospital of Southwest Jiaotong University, The Third People’s Hospital of Chengdu, 82 Qinglong St. Chengdu, 610015 Sichuan, P. R. China
†These authors contributed equally.
Academic Editor: Peter A. McCullough
Abstract
The burden of cardiovascular disease is predicted
to escalate in developing countries. The aim of this study
is to assess the characteristics, management strategies and outcomes of the
patients with acute coronary syndrome (ACS) who were admitted to hospitals under
the chest pain center mode in southwest P. R. China. Adults hospitalized with a diagnosis of ACS were enrolled in the retrospective,
observational registry between January 2017 and June 2019 at 11 hospitals in
Chengdu, P. R. China. The collected data included the patients’ baseline
characteristics, clinical management and in-hospital outcomes. After Statistical analysis,
(1) A total of 2857 patients with ACS, among which 1482 have ST-segment elevation
myocardial infarction (STEMI), 681 have non-STEMI (NSTEMI) and 694 have unstable
angina (UA) were enrolled in the study. (2) 61.3% of the ACS patients received
reperfusion therapy. More patients with STEMI
underwent percutaneous coronary intervention
(PCI) compared with NSTEMI/UA patients (80.6% vs. 38.8%, P
Keywords
- Acute coronary syndrome
- Clinical characteristics
- Percutaneous coronary intervention
- In-hospital outcomes
The prevalence and mortality of cardiovascular disease (CVD) in P. R. China is steadily increasing [1]. Acute coronary syndrome (ACS) is a common critical illness in CVD, which seriously endangers the people’s life and health and puts a great burden on the society.
The hospitals in P. R. China have been facing a series of challenges including the heavy burden of CVD, uneven geographical distribution of healthcare resources and weak inter-hospital collaboration for many years. Aiming to improve the treatment capability of chest pain patients, chest pain centers (standard and grassroots editions) have been actively constructed with a collaborative emergency system based on these centers, which contributes to improving the compliance with the ACS guidelines, optimizing the clinical pathways and improving the treatment procedures [2]. With the help of qualified chest pain centers, our study represents a Chinese multicenter clinical trial registration study that had established a typical collaborative emergency system, which was based on the foundation of the emergency medical system, an inter-hospital data transmission and the adoption of the optimal road map guiding for chest pain treatment among the enrolled hospitals.
No representative studies have been so far presented to define the clinical profiles, management and outcomes of ACS patients in southwest P. R. China. In order to improve the current understanding of ACS management, we sought to create an ACS registry from 2017 to 2019 to evaluate the presentation, management and outcomes of patients with ACS in Chengdu.
We established a retrospective multicenter registry that recruited patients with ACS from 11 tertiary hospitals, among which three are standard chest pain centers certified by the China Chest Pain Center headquarters, and eight are certified grassroots chest centers. An efficient and rapid two-way referral link has been established between the chest pain center and the primary hospital, and a regional collaborative treatment network has been established in Chengdu. This study included 2,857 ACS patients who were admitted to the above-mentioned hospitals from January 2017 to June 2019. The study was approved by the medical ethics committee of the Third People’s Hospital of Chengdu and its clinical trial registration number is ChiCTR1900025138.
Consecutive patients who were admitted to the hospital with ACS were enrolled at the centers, and their data at the time of admission were retrospectively recorded. The inclusion criteria were as follows: (1) being diagnosed with ST-segment elevation myocardial infarction (STEMI), non-STEMI (NSTEMI) or unstable angina (UA) [3], (2) aged 18 years or more. The patients with some missing clinical data or who did not know the treatment measures were excluded.
This is a retrospective study that collects the patient information obtained
from the hospital system. The data abstraction quality was monitored by random
auditing. The data recorded in the patient’s ACS registry included the
demographic characteristics, medical history, cardiovascular risk factors,
clinical characteristics, mode of transportation to the hospital, time of the
symptom onset, time of admission, first medical contact time,
time of start of the balloon (defined as the
time for the first balloon catheter dilation/aspiration of the thrombus. For
those who reached the blood flow of TIMI level 3 immediately after the passage of
the guidewire, the time to guidewire passage was recorded), treatments at the
hospital, findings of the diagnostic tests, length of stay at the hospital,
medical costs, discharge medications and outcomes at the hospital (death and
acute heart failure). Acute heart failure was defined as Killip class II and
above. Multivessel disease was defined as stenosis (
The SPSS statistical software (version 22.0) was used for the statistical
analysis. Dichotomous variables were presented as numbers and percentages and
compared using the
A total of 2857 patients were enrolled in the study and included in the
analysis, among which 1482 patients (51.9%) were diagnosed with STEMI, 681
patients (23.8%) with NSTEMI and 694 patients (24.3%) with UA. The baseline
characteristics of the participants are listed in Table 1. Among the entire
patient group, the mean age was (67
| Variable | N | STEMI 1482 | NSTEMI 681 | UA 694 | Total 2857 | P value |
| Demographic | ||||||
| Age (years) | 2854 (99.9%) | 66 ± 14 | 69 ± 13 | 67 ± 12 | 67 ± 13 | |
| Sex (male) | 2857 (100.0%) | 1105 (74.6%) | 463 (68.0%) | 452 (65.1%) | 2020 (70.7%) | |
| Cardiovascular risk factors | ||||||
| Hypertension | 2857 (100.0%) | 754 (50.9%) | 437 (64.2%) | 432 (62.2%) | 1623 (56.8%) | |
| Diabetes mellitus | 2857 (100.0%) | 352 (23.8%) | 188 (27.6%) | 186 (26.8%) | 726 (25.4%) | 0.101 |
| Dyslipidaemia | 2837 (99.3%) | 129 (8.8%) | 26 (3.8%) | 49 (7.1%) | 204 (7.2%) | |
| Current smoker | 2840 (99.4%) | 638 (43.4%) | 237 (35.0%) | 206 (29.8%) | 1081 (38.1%) | |
| Medical history | ||||||
| Myocardial infarction | 2829 (99.0%) | 38 (2.6%) | 33 (4.9%) | 69 (10.0%) | 140 (4.9%) | |
| Coronary heart disease | 2842 (99.5%) | 112 (7.6%) | 121 (17.8%) | 258 (37.3%) | 491 (17.3%) | |
| PCI | 2839 (99.4%) | 41 (2.8%) | 39 (5.8%) | 93 (13.5%) | 173 (6.1%) | |
| CABG | 2843 (99.5%) | 1 (0.1%) | 1 (0.1%) | 3 (0.4%) | 5 (0.2%) | 0.163 |
| Stroke | 2832 (99.1%) | 75 (5.1%) | 34 (5.0%) | 30 (4.4%) | 139 (4.9%) | 0.767 |
| Clinical characteristic | ||||||
| S-to-D (min) | 2852 (99.8%) | 190 (94, 468) | 283 (112, 1084) | 337 (97, 2220) | 226 (97, 758) | |
| Chest discomfort | 2748 (96.2%) | 1362 (94.5%) | 585 (88.8%) | 617 (95.2%) | 2564 (93.3%) | |
| Cardiac arrest | 2810 (98.4%) | 21 (1.4%) | 2 (0.3%) | 1 (0.1%) | 24 (0.9%) | 0.002 |
| Killip class | 2097 (96.9%) | |||||
| Killip class I | 861 (60.2%) | 480 (72.1%) | - | 1341 (63.9%) | ||
| Killip class II | 313 (21.9%) | 118 (17.7%) | - | 431 (20.6%) | ||
| Killip class III | 69 (4.8%) | 38 (5.7%) | - | 107 (5.1%) | ||
| Killip class IV | 188 (13.1%) | 30 (4.5%) | - | 218 (10.4%) | ||
| Heart rate (bpm) | 2813 (98.5%) | 78 (66, 91) | 78 (67, 90) | 74 (65, 85) | 76 (67, 90) | |
| Systolic blood pressure (mmHg) | 2823 (98.8%) | 128 |
137 |
138 |
132 |
|
| multivessel disease | 2052 (71.6%) | 805 (63.7%) | 294 (66.8%) | 162 (46.4%) | 1261 (61.5%) | |
| Tests | ||||||
| Glomerular filtration rate (mL/min) | 1811 (63.4%) | 81.8 |
81.5 |
89.0 |
83.9 |
0.182 |
| Troponin (ng/mL) | 1991 (69.7%) | 25.2 (5.1, 710.0) | 8.6 (1.87, 154.7) | 4.79 (0.4, 11.1) | 10.9 (1.9, 121.4) | |
| Hemoglobin (g/L) | 2665 (93.3%) | 133 |
129 |
132 |
131 |
|
| Transportation | 2857 (100.0%) | |||||
| Ambulances | 135 (9.1%) | 52 (7.6%) | 41 (5.9%) | 228 (8.0%) | ||
| Taxis/private cars | 857 (57.8%) | 481 (70.6%) | 598 (86.2%) | 1936 (67.8%) | ||
| Transfer | 456 (30.8%) | 118 (17.3%) | 45 (6.5%) | 619 (21.7%) | ||
| Hospital stay, days | 2818 (98.6%) | 9 (7, 11) | 8 (6, 11) | 8 (6, 11) | 9.0 (6, 11) | |
| Total costs, ten thousand yuan | 2818 (98.6%) | 3.98 (2.88, 5.14) | 2.38 (0.91, 4.34) | 1.02 (0.68, 1.76) | 3.21 (1.03, 4.58) | |
| P-value for three comparisons. STEMI, ST-segment elevation myocardial infarction. NSTEMI, non-STEMI. UA, unstable angina. PCI, percutaneous coronary intervention. CABG, coronary artery bypass grafting. S-to-D, the time from symptoms to hospital. Laboratory normal range troponin values is 0-5.0 ng/mL. | ||||||
60.4% of the patients underwent PCI (Table 2). The rates of coronary
angiography (CAG) and PCI were higher in patients with STEMI than in those with
NSTEMI/UA. However, thrombolytic therapy was used in only 1.8% of the STEMI
patients. Overall, almost all patients (98.3%) received antiplatelet drugs at
the hospital. Regarding the prescribed medication, lipid-lowering medication,
| Variable | STEMI 1482 | NSTEMI 681 | UA 694 | Total 2857 | P value |
| Coronary angiography | 1301 (87.8%) | 454 (66.7%) | 393 (56.6%) | 2148 (75.2%) | |
| No reperfusion | 262 (17.8%) | 335 (49.2%) | 507 (73.1%) | 1104 (38.6%) | |
| Fibrinolytic therapy | 26 (1.8%) | - | - | 26 (0.9%) | |
| PCI | 1194 (80.6%) | 346 (50.8%) | 187 (26.9%) | 1727 (60.4%) | |
| Primary PCI | 1068 (72.1%) | 190 (27.9%) | 46 (6.6%) | 1304 (45.6%) | |
| Drugs | |||||
| Single antiplatelet drugs | 75 (5.8%) | 79 (13.0%) | 204 (34.1%) | 358 (14.3%) | |
| Dual antiplatelet drugs | 1215 (93.4%) | 512 (84.3%) | 377 (63.0%) | 2104 (84.0%) | |
| lipid-lowering drugs | 1207 (95.9%) | 576 (94.3%) | 583 (93.9%) | 2366 (95.0%) | 0.116 |
| β-blockers | 870 (69.3%) | 418 (68.6%) | 394 (63.8%) | 1682 (67.7%) | 0.048 |
| ACEI/ARB | 627 (50.4%) | 361 (59.2%) | 352 (57.1%) | 1340 (54.3%) | 0.001 |
| P-value for three comparisons. STEMI, ST-segment elevation myocardial infarction. NSTEMI, non-STEMI. UA, unstable angina. PCI, percutaneous coronary intervention. ACEI, angiotensin-converting enzyme inhibitors. ARB, angiotensin receptor blockers. | |||||
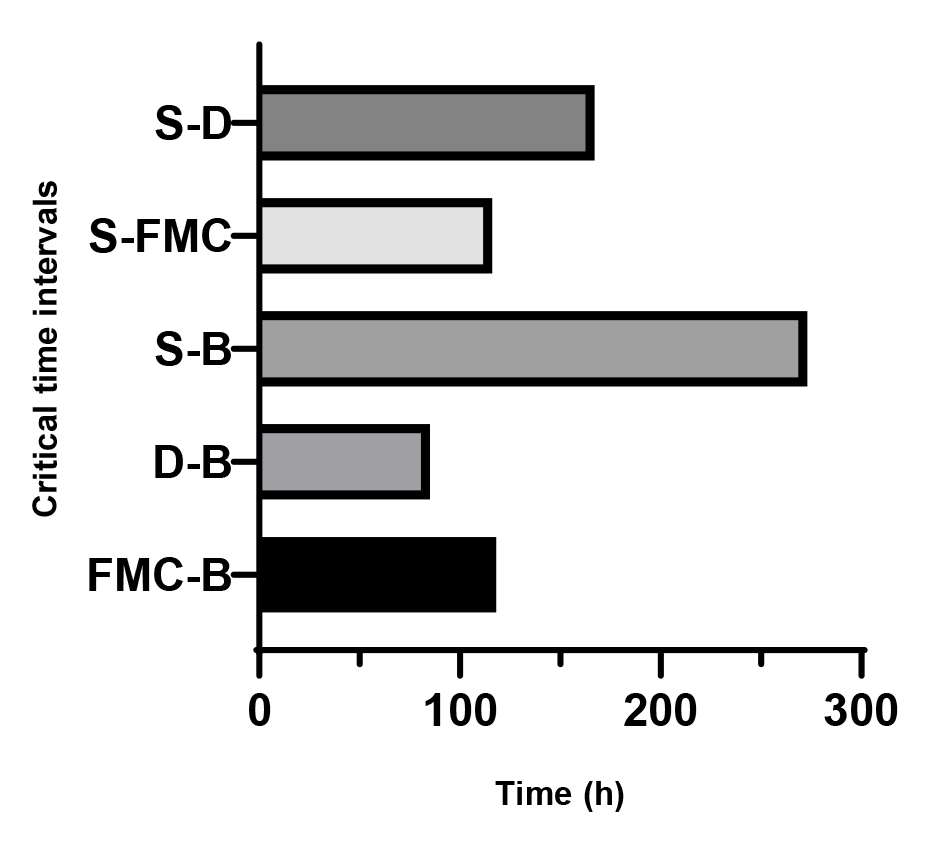
The critical time intervals of patients with STEMI for primary PCI are shown in Fig. 1 PCI was performed within 72 hours in 72.6% of NSTEMI and UA (NSTE-ACS) patients (Table 3).
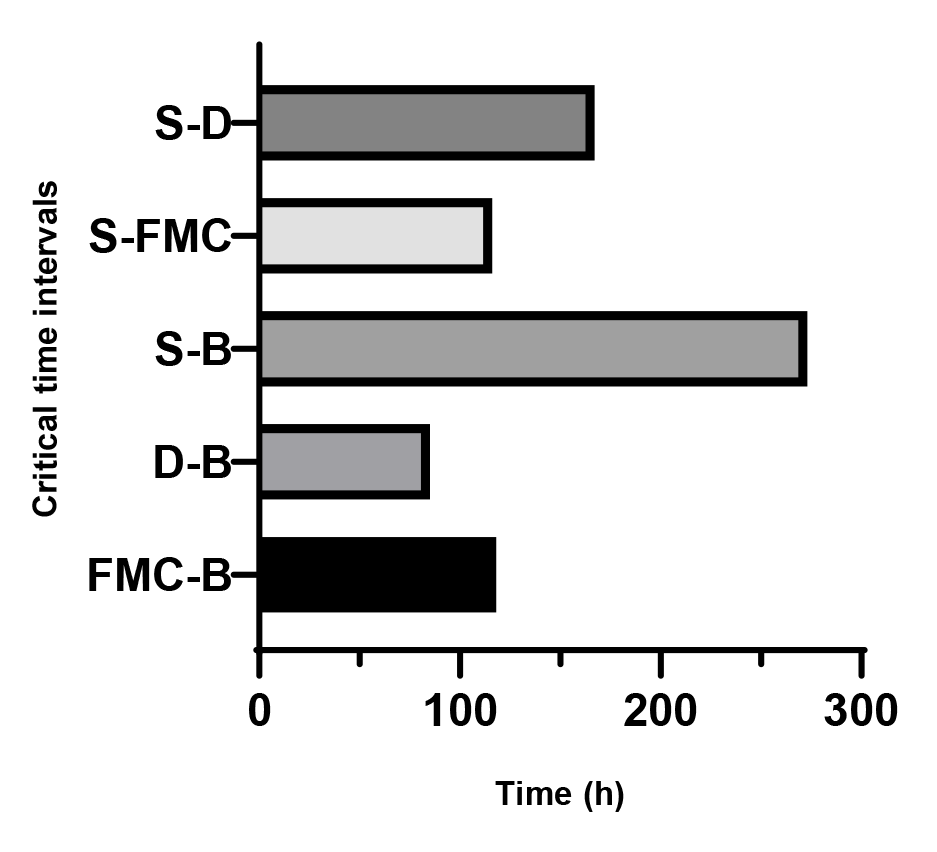 Fig. 1.
Fig. 1.Critical time intervals of patients with STEMI for primary PCI. S-D, the time from symptoms to hospital. S-FMC, the time from symptoms to first medical contact. S-B, the time from symptoms to start of the balloon. D-B, the time from door to start of the balloon. FMC-B, the time from first medical contact to start of the balloon.
| Variable | NSTEMI 681 | UA 694 | NSTE-ACS 1375 |
| Door-to-CAG time (h) | |||
| 85 (18.8%) | 33 (8.4%) | 118 (14.0%) | |
| 244 (54.1%) | 118 (30.2%) | 362 (43.0%) | |
| 349 (77.4%) | 266 (68.0%) | 615 (73.0%) | |
| Door-to-PCI time (h) | |||
| 58 (16.9%) | 4 (2.2%) | 62 (11.7%) | |
| 189 (54.9%) | 46 (24.9%) | 235 (44.4%) | |
| 267 (77.6%) | 117 (63.2%) | 384 (72.6%) | |
| The proportion of interventional patients in angiography (%) | 76.2 | 47.6 | 62.9 |
| NSTE-ACS, NSTEMI and UA. | |||
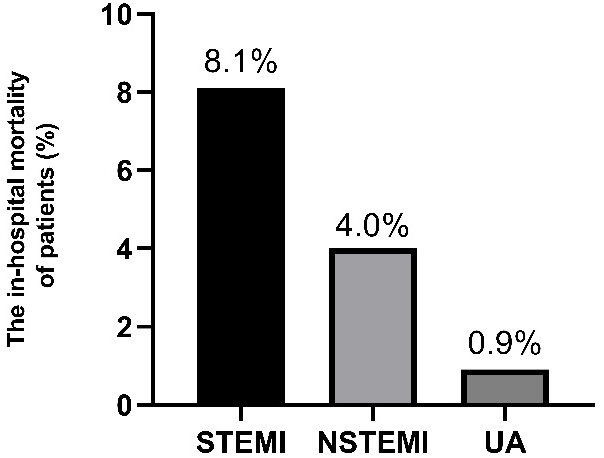
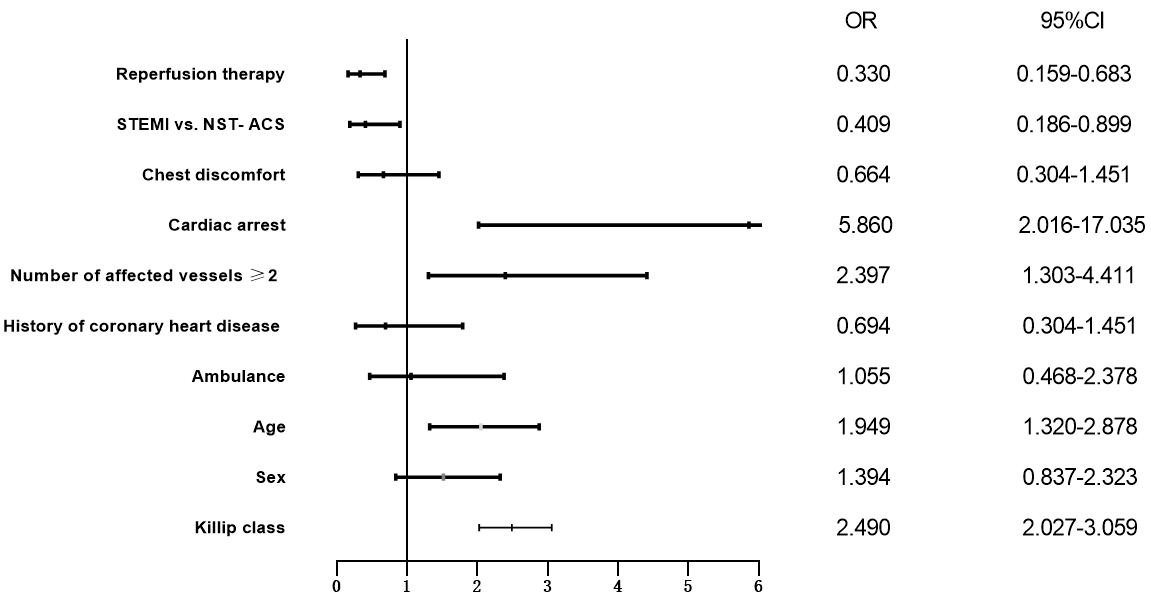
The in-hospital outcomes for patients with ACS
were death (5.4%) and acute heart failure (17.8%), as listed
in Fig. 2 and Table 4. After logistic regression analysis, independent prognosticators of in-hospital mortality in ACS patients were: STEMI, cardiac arrest, number of affected vessels
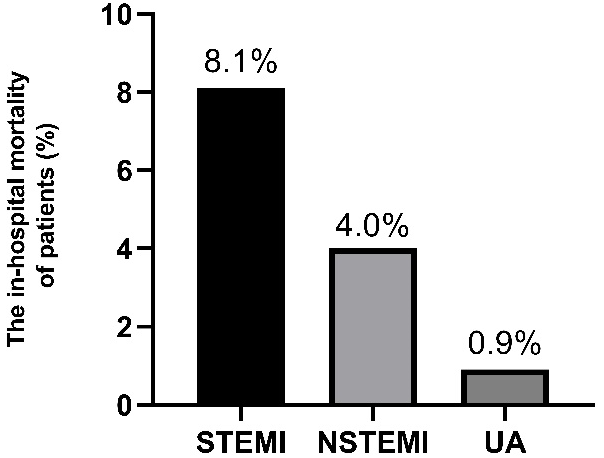 Fig. 2.
Fig. 2.The in-hospital mortality of patients with ACS. The in-hospital mortality for patients with STEMI was 8.1%. Outcomes for those with NSTEMI/UA were 4.0% and 0.9%.
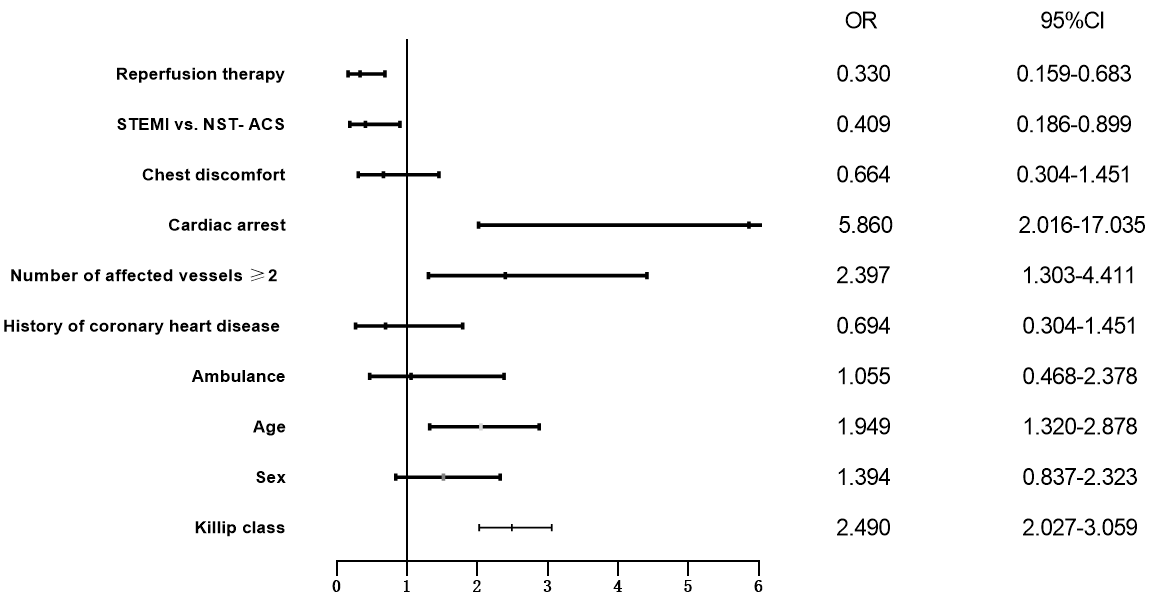 Fig. 3.
Fig. 3.Logistic regression analysis was used to identify independent predictors of hospital mortality. After logistic regression analysis, independent prognosticators of in-hospital mortality in ACS patients
were: STEMI, cardiac arrest, number of affected vessels
| Variable | STEMI 1482 | NSTEMI 681 | UA 694 | Total 2857 | P value |
| Acute heart failure | 327 (22.6%) | 100 (15.3%) | 67 (9.9%) | 494 (17.8%) | |
| Death | 120 (8.1%) | 27 (4.0%) | 6 (0.9%) | 153 (5.4%) | |
| Death or Acute heart failure | 363 (25.0%) | 110 (16.8%) | 68 (10.1%) | 541 (19.4%) | |
| P-value for three comparisons. | |||||
This study was conducted to document the baseline information, management strategies and in-hospital mortality of the patients admitted to hospitals with a diagnosis of ACS in Chengdu, P. R. China. In contrast to the data reported from developed countries [4, 5], we recorded more cases of STEMI than NSTEMI or UA. Patients with STEMI tended to be slightly younger than those with NSTE-ACS, with a higher proportion of men, fewer risk factors and a less frequent history of cardiac disease. However, they were more often smokers and had a higher all-cause mortality rate.
Early revascularization leads to a significant reduction in cardiovascular events [6]. As an important treatment for ACS, PCI contributes to a favorable prognosis. The rate of STEMI patients undergoing PCI was much higher in our registry (79.7%) than in previous studies in P. R. China [7, 8, 9] and the rate of primary PCI (pPCI) in STEMI patients was 72.1%, which is comparable to the percentage of 70-80% in European and American countries [10] and significantly higher than the percentages of pPCI patients in 2017 and 2018 published by the National Center for Cardiovascular Health Quality Control in mainland P. R. China (42.2% and 45.94%, respectively). The high proportion of STEMI patients with pPCI in Chengdu indicates that the construction of chest pain centers contributes to improving the medical level and quality of services provided by the hospitals. As a result, the treatment of STEMI patients has better outcomes, which is conducive to improving the prognosis of the patients. It was found that although the in-hospital mortality of patients with NSTEMI or UA may be lower than that of patients with STEMI, the mortality rate was already comparable to that of STEMI patients at 1 and 2 years of follow-up after being discharged, reflecting the importance of clinical treatment in NSTEMI and UA [11, 12].
In this study, the proportion of patients with NSTE-ACS receiving CAG (60.9%) was comparable to the percentage published by the previous Care for Cardiovascular Disease in China (CCC) study (63.1%) [13], but only 38.8% of the patients received PCI, far lower than the percentage of 58.2% in the CCC study. Besides, the proportion of patients who underwent CAG and PCI was lower than that of the developed countries [4, 14]. The proportion of patients with NSTEMI/UA who underwent PCI was even less than half of that of STEMI patients (79.7%), and the proportion of NSTEMI/UA patients who underwent CAG was also lower than that of STEMI patients. This might be because STEMI is more critical, and it also indicates that doctors pay less attention to patients with NSTEMI/UA and the management in those cases is not as active as in STEMI cases. In addition, clinicians should enhance the awareness of symptoms among NSTEMI/UA patients.
Overall, 61.3% of the ACS patients in this study received revascularization, 60.4% of which were PCI, up from two-fifths of the patients as reported in the GRACE registry [15] but there was still room for improvement compared with the PACIFIC registry in Japan [16]. Our thrombolytic rate was the lowest compared with other similar studies [7, 8, 14], this might be because PCI is considered as the main treatment of reperfusion and the current national guidelines list pPCI as the preferred treatment for acute MI. Besides, the study included secondary and tertiary hospitals, some of which are still mainly venous thrombosis treatment hospitals (especially primary hospitals) that were not included, which may underestimate the proportion of thrombosis in Chengdu.
The median time from symptom onset to hospital admission in STEMI (190 min) was better compared with previous studies conducted in P. R. China [7, 8], which may be due to the economic growth and overall development that led to an increase in the public awareness of medical treatment. However, patients with STEMI in our study took much longer to reach the hospital than the patients in developed countries (145 minutes in Germany [17] and 141 minutes in France [18]) and this could be improved. In this study, patients with NSTEMI/UA took even longer to reach the hospital, which was also demonstrated in several other large-scale studies [14, 18, 19]. Possible explanations include that NSTEMI patients were more likely to present without typical symptoms (chest pain, palpitation and dyspnea), and they tend to be older with more comorbidities including hypertension and DM, so identifying the symptoms of cardiac origin may be masked by these chronic diseases and pre-hospital delays. Our results were useful for both clinicians and patients to gain a deeper understanding of the symptoms of NSTEMI and to reduce pre-hospital delays.
The door-to-balloon time (D-B) for primary PCI was 85 min in STEMI patients, which complied with the domestic and international guidelines for the recommended D-B within 90 minutes. However, there was still a gap compared with the developed countries (63 minutes in the United States [16], 50 minutes in Germany [17] and 68 minutes in South Korea [20], and the compliance rate of having D-B within 90 minutes was only 56.8%, far lower than the standard set by the Chinese Chest Pain Center (75%)). Common reasons for delays in the D-B include delays in catheter lab access, activating catheter lab team and transfer, as well as financial reasons and having a long queue of patients, all these factors should be addressed [21]. The establishment of the chest pain center aims to optimize the treatment process of ACS and reduce the reperfusion time. In addition, the national medical security system needs to be further improved.
In this study, the in-hospital mortality of the STEMI patients was comparable to that of the European and American countries (4%-12%) [4], but there was no significant decline compared with the China PEACE-Retrospective Acute Myocardial Infarction Study (China PEACE study) [7], this may be due to the higher incidence and worse condition of the cardiogenic shock in STEMI patients in this study, which lead to a poor prognosis. Although the median time from symptoms to hospital in this study was shorter than that in the China PEACE study [7], the reperfusion time of some patients was delayed after admission, and the total myocardial ischemia time was slightly longer, which may lead to a higher mortality. Moreover, there is still space for improvement in the PCI rate of STEMI patients compared with developed countries (95.6% in Japan [22]). The lower proportion of NSTEMI/UA patients with PCI in this study compared with the CCC study may have contributed to the slightly higher in-hospital mortality rate in this study (2.4%) compared with the CCC study (1.7%) [13]. In this study, the incidence of acute heart failure and shock in NSTE-ACS patients was higher than that in CCC [13], and patients had a relatively worse prognosis. Therefore, reducing the in-hospital mortality may be achieved by raising the awareness of the disease symptoms, reducing the pre-hospital patient delay and receiving the medical care as soon as possible, i.e., reducing the total myocardial ischemia time of the patients.
The purpose of secondary prevention of ACS is to reduce the recurrence of MI and
improve the patients’ quality of life. As a result, the guidelines [23] recommend
treating ACS patients with antiplatelet drugs, beta-blockers,
ACEI/ARB and statins after being discharged,
as well as applying lifestyle and health education interventions.
In our study, the utilization rates of the
antiplatelet drugs and statins were high, better than those in developed
countries such as Japan [22], but the rate of using
Most of the patients were transferred to hospitals by private vehicles instead
of ambulances, which has been associated with pre-hospital delays and may lead to
an increased probability of cardiac arrest. Another important act to consider is
to provide better education to the public by the health care professionals,
especially to people at a high risk of ACS, to help them recognize that
ambulances are not only simple transportation vehicles but “mobile hospitals”
for early diagnosis and rescue of critical illnesses. In our study, the median
hospital stay length was 8 days for NSTEMI/UA patients, longer than the reported
median of 3 to 4 days in the United States or European countries [24, 25], this
might be because a much smaller proportion of the patients received early PCI in
our study compared with the United States or European countries, with about
30.0% of the patients receiving PCI
The findings of this study should be interpreted in view of several limitations. Firstly, the prospective nature of this study may have caused some degree of bias during data collection. Secondly, our study was an observational non-randomized registry, which may be subjected to selection bias that is related to this type of clinical investigations. Finally, 11 participating hospitals were secondary or tertiary hospitals with facilities for advanced interventional therapy, which may overestimate the proportion of performed PCI and underestimate the proportion of applied thrombolytic therapy in ACS patients in Chengdu.
Management of ACS has improved significantly in Chengdu, P. R. China owing to the construction of chest pain referral centers with a collaborative emergency system. However, important gaps continue to persist in terms of outcomes when compared to developed countries. Awareness among physicians and patients may help further improve outcomes and efficiency in the management of ACS.
All authors have contributed significantly. Si-Yi Li and Ming-Gang Zhou contributed to the conception of the work, literature search, experimental studies, data acquisition, data analysis, manuscript preparation, manuscript editing. And Si-Yi Li was a major contributor to the writing of the manuscript. Tao Ye and Lian-Chao Cheng contributed to the conception of the work, manuscript review and approval of the final version of the manuscript. Feng Zhu, Cai-Yan Cui and Yu-Mei Zhang contributed to experimental studies, literature search and data acquisition. Lin Cai contributed to the design, literature search, experimental studies, manuscript review, approval of the final version of the manuscript, and agreement of all aspects of the work.
The study was approved by the Medical Ethics Committee of The Third People’s Hospital of Chengdu (Ethics approval number: Chengdusanyuanlun [2019] S-67), where exempted informed consent from enrolled patients because of retrospective study protocol.
The authors thank all participants for their help and are grateful for the resources provided by the hospital. Thanks to all the peer reviewers and editors for their opinions and suggestions. We also thank EditSprings (https://www.editsprings.com/) for its language help during the preparation of this manuscript.
This study was supported by Applied Basic Research Project in Sichuan Province (No. 2018JY0126).
The authors have no conflicts of interest to declare.