Academic Editors: Giuseppe Biondi-Zoccai and Dragan M. Djuric
The stress management program is not considered as a part of routine cardiac rehabilitation due to the lack of consensus and inconsistencies in the studies detailing the relation between stress and coronary artery disease. The current meta-analysis is intended to determine the effectiveness of stress management in cardiac rehabilitation. The published literature studies until December 2020 were extracted from various databases and eligible studies were selected based on the inclusion and exclusion criteria. Quality assessment of the selected studies was carried out using Jadad. The literature search of various databases yielded 154 studies and 9 were selected based on the inclusion/exclusion criteria. On the Jadad scale, 6 studies obtained a score of 3, whereas the remaining studies obtained a score of 2. Funnel plot findings reported no publication bias. The result of the meta-analysis showed a persistent improvement in Beck depression inventory-2, hospital anxiety scale and hospital depression scale in subjects who had undergone various stress management interventions. The meta-analysis corroborates the benefits of stress management training in cardiac rehabilitation and underscores the need to adopt a stress management program in routine cardiac care.
The health and economic burden of cardiovascular disease (CVD) are substantial, and it is the leading cause of global mortality and disability [1]. As per the Global Burden of Disease (GBD) Study there is a 2-fold increase in the prevalence of CVD from 271 million in 1990 to 523 million in 2019. Similarly, there is a 2-fold increase in the disability-adjusted life years (DALYs) and years of life lost over that period. The CVD-related mortality noted in the corresponding years was 12.1 million and 18.6 million [2]. There is substantial literature evidence to validate the role of psychosocial factors such as stress, depression and anxiety in contributing to the onset, progression and prognosis of coronary heart diseases (CAD). Physical and emotional effects of stress may in turn contribute to the release of certain hormones that increase hypertension, thereby enhancing the clotting of arteries. The build-up of fatty material called atheroma can cause angina, myocardial infarction (MI) or sudden death [3]. Since both acute and chronic stress play a leading role in the development and progression of CAD, stress management involving combined education, group support, and cognitive-behavior therapy is advocated to improve cardiac health in CAD and MI patients.
Despite the extensive epidemiological literature evidence validating the beneficial effects of stress management in improving cardiac health, it is not included as a part of routine cardiac rehabilitation (CR). The stress management interventions are not offered as a part of routine CR could be due to the lack of consensus about the most effective approach and stress quantification, and inconsistencies in the studies detailing the association between stress and CAD [4].
Over the past few decades, cardiac rehabilitation has evolved as a multidisciplinary approach that focuses on customized exercise training, patient education, modification of risk factors and the overall well-being of cardiac patients [5]. Recently, there is a greater emphasis on the management of psychological, nutritional, behavioral and social factors, which can influence the patient outcomes [6]. A randomized clinical trial by Blumenthal et al. [4] has concluded that stress management training may confer an incremental benefit upon combining with comprehensive cardiac rehabilitation. Cognitive behavioral therapy focusing on coping skills has shown to help patients to deal with physical/functional changes and heart failure associated sequelae by promoting adaptation, a positive health attitude, and decreasing the psychological burden [7]. Exercise has been shown to provide various health benefits in patients with heart failure. It helps in a partial reversal of underlying skeletal muscle changes, which contribute to worsening of heart failure and associated symptoms and improving physical function and health-related quality of life (HRQOL) [8].
Various instruments are used for assessing the stress-related symptoms, determining possible treatment options, and gauging their progress to guide the treatment. Many of these instruments have been used in studies that serve as an evidence base for systematic reviews and developing treatment recommendations [9]. The instruments considered in the current meta-analysis include stress behavior score, heart-focused anxiety (HAF-17), quality of life (QoL), Beck depression inventory (BDI)-2, hospital anxiety scale (HAS), and hospital anxiety and depression scale (HAD).
The present review and meta-analysis are aimed to determine the effectiveness of stress management among CAD and MI patients. Compiling the literature findings through meta-analysis may help in validating the relationship between stress and CAD, thereby including stress management as a part of routine cardiac rehabilitation programs.
The review was planned and conducted in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [10]. Relevant studies were retrieved from the various electronic databases and were included based on the criteria and eligibility.
The published literatures until December 2020 were extracted from the databases namely PubMed, Cochrane, Google Scholar, Embase and Scopus. The keywords considered for the search were ‘stress management’, ‘effectiveness’, ‘cardiac rehabilitation’, ‘coronary artery disease’, ‘cognitive behavioral therapy’, ‘ischemic heart disease’, ‘coronary atherosclerosis’, ‘coronary arteriosclerosis’, ‘myocardial infarction’, ‘heart attack’ and ‘cardiovascular rehabilitation’. Randomized control trials, case-control/cross-sectional studies and intervention studies dealing with stress management during cardiac rehabilitation were included. Hospital record-based or single center-based retrospective studies were excluded. The studies with the outcomes based on psychosocial stress measures, CAD biomarkers, and lipid profile parameters were included in the study. The exclusion criteria considered were inappropriate interventions and outcomes (negative or small effects with lack of data), abstracts, reviews, animal studies and case reports; non-English articles; studies with insufficient protocol (insufficient data, compliance and lack of clarity related to procedure); articles with required pages missing; studies discussing stress management methods other than cognitive behavioral therapy; studies on exercise therapy used as cardiac rehabilitation; and non-randomized, retrospective, and home-based studies.
The reviewers investigated and extracted data from selected and eligible studies. Major outcomes considered for data extraction were psychosocial stress measures, CAD biomarkers, and lipid profile parameters. Fig. 1 shows the flow diagram of the study selection.
 Fig. 1.
Fig. 1.PRISMA flow diagram of the screening procedure and study selection.
The quality assessment of the studies selected for inclusion was carried out
using the Jadad score [11]. The Jadad score comprised of three items:
randomization (0–2 points), blinding (0–2 points), and dropouts and withdrawals
(0–1 points). The response to each item was marked as “yes” (1 points) or
“no” (0 points). The final score ranged from 0 to 5 points, with higher scores
indicating better reporting. Studies with a Jadad score of
The chances of publication bias were measured through visual representation using a funnel plot with the y-axis representing the standard error (SE) of each study and the x-axis representing the arcsine-transformed proportion of each study.
A systematic review of the literature was conducted with the help of Rayyan
systematic review and Zotero software (George Mason University, Virginia, USA).
Meta-analysis was carried out as fixed effect and random effects models using R
opensource software (R Foundation for Statistical Computing, Vienna, Austria).
The packages of R used for meta-analysis were metafor, meta and
qdap. Visual representation of meta-analysis was depicted using Forest
plots. The impact of the model was picked relying upon the level of heterogeneity
(I
The literature search of various databases yielded 154 studies until December 2020. Based on the inclusion/exclusion criteria, 9 studies were selected by the experts for meta-analysis and 98 studies were excluded. The reasons for exclusion and the number of papers excluded are brief below: inappropriate interventions and outcomes, abstracts, reviews, animal studies and case reports (n = 10), non-English articles (n = 8), an insufficient protocol for studies (n = 8), required pages missing in articles (n = 6), stress methods other than cognitive behavioral therapy (n = 23), exercise therapy used as cardiac rehabilitation (n = 20), non-randomized, retrospective, home-based, and descriptive qualitative studies (n = 17), and non-availability of post-treatment values in papers (n = 6) (Fig. 1).
Table 1 (Ref. [13, 14, 15, 16, 17, 18, 19, 20, 21]) lists the baseline characteristics of the final 9 studies that were selected for inclusion. A total of 4 studies [13, 15, 17, 20] were reported from Sweden and 2 from Germany [16, 19] and USA [14, 21] and one from Singapore [18]. There are three studies were conducted only among female subjects [13, 15, 20] compared to a study with male subjects only [17]. Most of the studies conducted the stress management program based on combined education, group support, and cognitive behavioural therapy (CBT), skills training, and self-monitoring. The psychosocial effect was measured using BDI 2, CBT, HAD, and HAS scale scores among the subjects in the selected studies and reported in Table 2 (Ref. [13, 14, 15, 16, 17, 18, 19, 20, 21]) as baseline and after the post-treatment. In most of the studies, the subjects were followed up to a year and a minimum of 4 weeks to understand the outcomes from the stress management program (Table 3, Ref. [13, 14, 15, 16, 17, 18, 19, 20, 21]). Mostly there were no deaths during the follow-up period except a study reported in Sweden by Koertge, 2008 [20].
| No. | Study design | Author | Study site | Stress management | Study group | Psychosocial measures | Age (years) | Gender |
| Mean (SD) | ||||||||
| 1 | Randomized control | Blom et al., 2009 [13] | Sweden | combined education, group support, and CBT, skills training, Self-monitoring | intervention | Self-rated daily Stress Behavior | 61.5 (8.9) | female = 113 |
| control | 62.5 (8.7) | female = 122 | ||||||
| 2 | Randomized control | Blumenthal et al., 2016 [14] | USA | combined education, group support, and CBT, skills training, Self-monitoring + comprehensive CR | intervention | BDI-2 | 61.8 (10.8) | female = 31, male = 45 |
| control | 60.9 (9.1) | female = 28, male = 49 | ||||||
| 3 | Randomized control | Karlsson et al., 2007 [15] | Sweden | physical training + cooking and counseling about diet + CBT | intervention | HAD | 63.8 (7.2) | female = 22 |
| control | HAS | 63.3 (7.3) | female = 30 | |||||
| 4 | Randomized control | Michalsen et al., 2005 [16] | Germany | CBT, combined education, group support, spiritual development, skills training, Self-monitoring, meditation | intervention | BDI-2 | 59 (8.7) | male = 38 |
| control | QoL | 59.8 (8.6) | male = 40 | |||||
| 5 | Randomized control | Sundin et al., 2003 [17] | Sweden | combined education, group support, and CBT, skills training, Self-monitoring, cooking, spiritual development | Multifactorial intervention | BDI-2 | 58.8 (7.2) | male = 33 |
| Multifactorial intervention | 57.6 (6) | male = 31 | ||||||
| Stress focused intervention | HAS | 58.8 (7.2) | male = 32 | |||||
| control | 58.9 (7.9) | male = 33 | ||||||
| 6 | Randomized control | Wang et al., 2018 [18] | Singapore | combined education, group support, and CBT, skills training | intervention | HAD | 60.8 (8.32) | female = 6, male = 59 |
| control | HAS | 60.8 (9.33) | female = 8. male = 56 | |||||
| 7 | Randomized control | Lena et al., 2019 [19] | Germany | combined education, group support, and CBT, skills training, self-monitoring, therapeutic techniques | intervention | HAS | 65 (7.99) | female = 3, male = 17 |
| control | 65.7 (8.88) | female = 3, male = 17 | ||||||
| 8 | Randomized control | Koertge et al., 2008 [20] | Sweden | combined education, group support, CBT, skills training, Self-monitoring | intervention | BDI-2 | 61.36 (9.1) | female = 119 |
| control | 62.73 (8.72) | female = 128 | ||||||
| 9 | Randomized control | Blumenthal et al., 2005 [21] | USA | combined education, group support, and CBT, skills training, self-monitoring, therapeutic techniques | intervention | BDI-2 | 63 (11.5) | female = 15, male = 29 |
| control | 63 (9) | female = 10, male = 32 | ||||||
| BDI, Beck depression inventory; CBT, cognitive behavioural therapy, HAD, Hospital Anxiety and Depression Scale; HAS, Hospital Anxiety scale; QoL, Quality of Life. | ||||||||
| References | Study group | BDI-2 | QoL | Daily stress behavior score | Hospital Depression Scale | Hospital Anxiety Scale | HAF-17 | ||||||
| mean (SD) | mean (SD) | mean (SD) | mean (SD) | mean (SD) | mean (SD) | ||||||||
| Baseline | Post-treatment | Baseline | Post-treatment | Baseline | Post-treatment | Baseline | Post-treatment | Baseline | Post-treatment | Baseline | Post-treatment | ||
| Blom et al., 2009 [13] | Intervention | 39.5 (8.1) | 36.1 (7.2) | ||||||||||
| Control | 37.2 (9.1) | 35.9 (8.5) | |||||||||||
| Blumenthal et al., 2016 [14] | Intervention | 8.1 (7.7) | 5 (2.1) | ||||||||||
| Control | 8 (8.2) | 7.1 (6.2) | |||||||||||
| Karlsson et al., 2007 [15] | Intervention | 8 (3.4) | 6.7 (3.1) | 6.8 (3) | 5.3 (3) | ||||||||
| Control | 9.4 (4.4) | 8.4 (4) | 7.2 (3.6) | 6.6 (3.8) | |||||||||
| Michalsen et al., 2005 [16] | Intervention | 9.3 (6.3) | 6.4 (4.2) | 3.3 (0.9) | 2.8 (0.8) | ||||||||
| Control | 9.8 (5.8) | 7.6 (4.7) | 3.5 (2) | 2.2 (1) | |||||||||
| Sundin et al., 2003 [17] | Residential multifactorial intervention | 10.3 (1.3) | 8.4 (2) | 6.1 (4) | 3.9 (2) | ||||||||
| Outpatient, multifactorial intervention | 7.6 (1.6) | 6.1 (2) | 4.2 (3.1) | 3.4 (1.1) | |||||||||
| Outpatient, stress focused intervention | 6.6 (1.8) | 6.6 (1) | 3.6 (2.1) | 2.2 (1) | |||||||||
| Control | 8.7 (1.6) | 7.1 (1) | 5.7 (3.2) | 4.2 (1.2) | |||||||||
| Wang et al., 2018 [18] | Intervention | 2.88 (3) | 1.21 (1) | 3.11 (3.48) | 1.81 (2.10) | ||||||||
| Control | 3.23 (2.92) | 2.90 (2) | 3.63 (3.73) | 2.23 (2.32) | |||||||||
| Lena et al., 2019 [19] | Intervention | 1.46 (0.36) | 1.09 (0.3) | ||||||||||
| Control | 1.22 (0.52) | 1.2 (0.4) | |||||||||||
| Koertge et al., 2008 [20] | Intervention | 11.2 (6.2) | 9.8 (6) | ||||||||||
| Control | 10.7 (7.1) | 9.5 (6.8) | |||||||||||
| Blumenthal et al., 2005 [21] | Intervention | 9.5 (8) | 4.2 (3.1) | ||||||||||
| Control | 8.9 (7.9) | 6.3 (5.4) | |||||||||||
| BDI, Beck depression inventory; HAF, Heart-focused anxiety; QoL, Quality of Life. | |||||||||||||
| References | Follow-up period | Deaths | Outcomes |
| Blom et al., 2009 [13] | 1–2 years | No deaths have been reported | Reduced self-rated daily stress behavior over time, results partly reflects regression toward the mean effects |
| Blumenthal et al., 2016 [14] | 5.3 years (median, 3.2 years; interquartile range, 2.2, 4.3 years | No deaths have been reported | Patients in the CR+SMT group reported reduced symptoms of anxiety, depression, and stress and had better clinical outcomes |
| SMT could be beneficial for all cardiac patients and suggest that SMT should be incorporated into comprehensive CR | |||
| Karlsson et al., 2007 [15] | 1-year | No deaths have been reported | Reduced type D score, anxiety and depressive symptoms and improves quality of life in coronary artery disease patients |
| Michalsen et al., 2005 [16] | 1-year | There were no deaths during the study | Depression, anxiety, anger and perceived stress were reduced |
| Sundin et al., 2003 [17] | 1-year | No deaths have been reported | Standard care of today appears to have great potential when changing lifestyle, in particular, if supplemented with some sort of stress management impact of prolonged follow-up periods of psychosocial interventions is needed |
| Wang et al., 2018 [18] | 4 weeks and 16 weeks | No deaths have been reported | There was no significant effect on self-management cardiac rehabilitation program among the outpatients with coronary heart disease. |
| Lena et al., 2019 [19] | 6 months | No deaths have been reported | BCC strategy is well accepted by patients, and feasible in the German healthcare system. It appeared effective in reducing risk factors in CAD patients |
| Koertge et al., 2008 [20] | 1–2 years | 1 (died between randomization and baseline examination), and 1 (died after the intervention period) | The stress management program among CAD women experienced a more pronounced decrease in vital exhaustion than controls |
| 2 (died between baseline and 10 week examination), 4 (between 10 weeks and 1 year), and 3 (between 1 year and end of follow-up) | |||
| Blumenthal et al., 2005 [21] | 16 weeks | No deaths have been reported | Stress management training offer considerable promise to patients with stable IHD through improvement in psychosocial adjustment and by modification of disease risk markers that may translate into improved clinical outcomes |
| BCC, Blended collaborative care; CAD, Coronary heart disease; CR, cardiac rehabilitation; IHD, Ischemic heart disease; SMT, self-monitoring therapy. | |||
The quality assessment of selected studies was performed using the Jadad score.
The detailed results are presented in Table 4 (Ref. [13, 14, 15, 16, 17, 18, 19, 20, 21]). Using the Jadad
scale, 6 studies obtained a score of 3, whereas the remaining studies obtained a
score of 2. There was no publication bias as depicted in funnel plots as the
number of studies are less than
| Study | Randomized control study | Sequence of randomization described and appropriate | Double-blind study | Method of double blinding described and appropriate | Withdrawals and dropouts | Sequence of randomization described and inappropriate | Double-blind method described and inappropriate | Jadad scores |
| Blom et al., 2009 [13] | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 3 |
| Blumenthal et al., 2016 [14] | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 2 |
| Karlsson et al., 2007 [15] | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 3 |
| Michalsen et al., 2005 [16] | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 3 |
| Sundin et al., 2003 [17] | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 3 |
| Wang et al., 2018 [18] | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 2 |
| Lena et al., 2019 [19] | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 3 |
| Koertge et al., 2008 [20] | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 2 |
| Blumenthal et al., 2005 [21] | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 3 |
The meta-analysis considered 5 studies that assessed the BDI-2 baseline. The
analysis showed that inconsistency was less among the studies
(
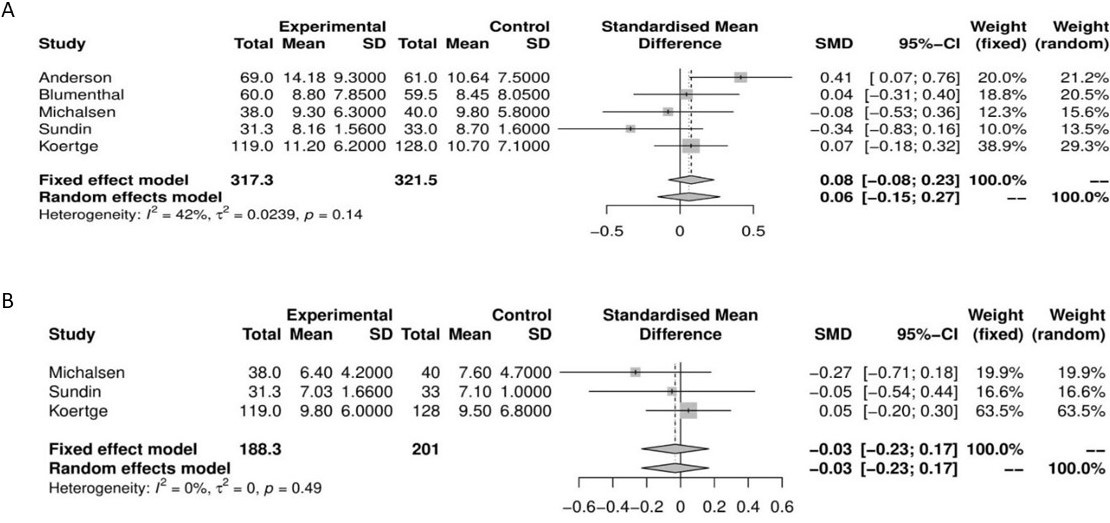 Fig. 2.
Fig. 2.Forest plot showing the standardized mean difference. The effective size for BDI-2 baseline (A) and post-treatment (B).
For hospital anxiety scale baseline, 4 studies were considered and the
meta-analysis showed that the inconsistency was nil among the studies
(
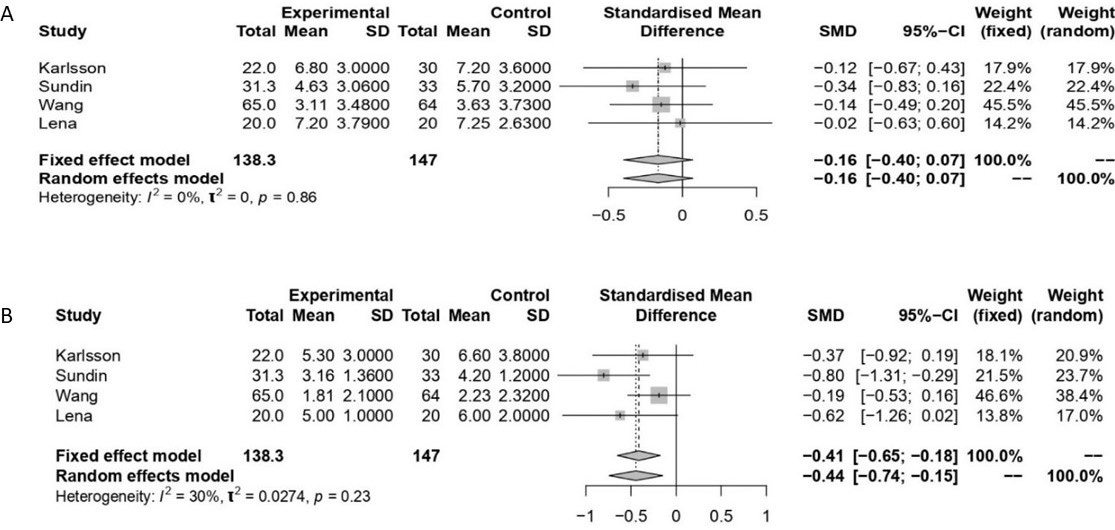 Fig. 3.
Fig. 3.Forest plot showing the standardized mean difference. The effective size for hospital anxiety scale baseline (A) and post-treatment (B).
Two studies that had assessed the hospital depression scale at baseline were
considered for meta-analysis and the inconsistency was nil among the studies
(
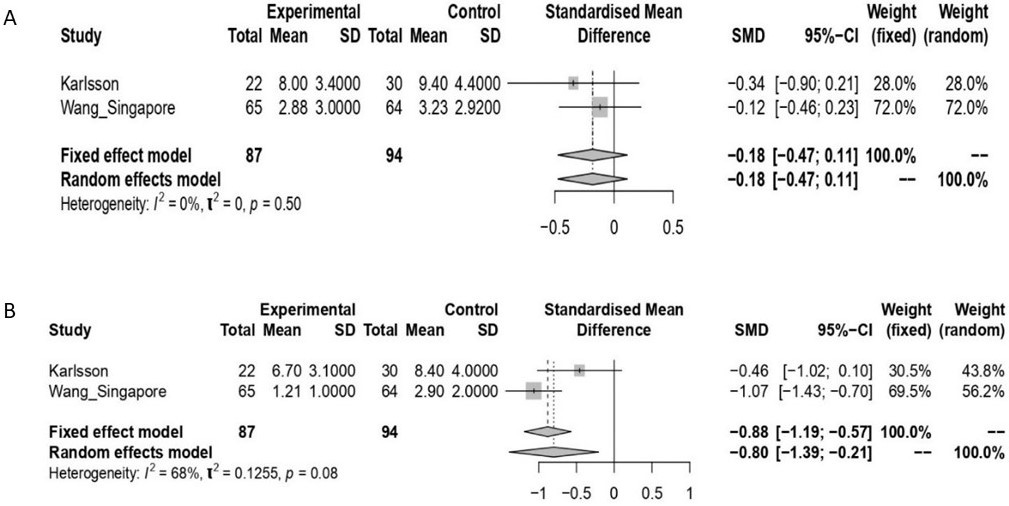 Fig. 4.
Fig. 4.Forest plot showing the standardized mean difference. The effective size for hospital anxiety and depression scale baseline (A) and post-treatment (B).
The stress management program at baseline and post-treatment for the aforementioned variables indicate a significant reduction in stress and anxiety compared to the comparator arms. Since only one study was available for either baseline or post-treatment, a meta-analysis was not carried out for daily stress behavior score, HAF-17, and QoL.
The present meta-analysis corroborates the significance of stress management in
cardiac rehabilitation. The study has noted a persistent improvement in BDI-2
[14, 16, 17, 20, 21], HAS [15, 17, 18, 19] and HAD [15, 18] scale in subjects who had
undergone various stress management interventions. In concurrence with the
current findings, a previous clinical trial by Blumenthal et al. [22] has reported
that stress-management or exercise training had conferred better clinical
outcomes in CAD patients having ischemia induced by mental stress. Stress
management was linked to reduce ischemia-induced by mental stress and relative
risk for at least 1 cardiac event during a follow-up period of 38 months was
found to be 0.26 compared to the controls [22]. Similarly, a randomized
controlled trial involving 201 African American men and women with CAD, conducted
for
Several international guidelines and position papers underscore the need for screening of stress and psychosocial risk factors, and adoption of various psychological interventions programs such as counseling, psychotherapy motivational interviews, and health psycho-education as a part of cardiovascular rehabilitation and prevention [24]. A position paper published by the German Cardiac Society has highlighted the relevance of psychosocial factors in cardiological care and advocated a multimodal treatment concept comprising of education, motivational counseling physical exercise, relaxation training and stress management [25].
A systematic and meta-analysis by Albus et al. [26] evaluated 20
studies published between January 1995 and October 2017 to analyze the additional
effects of psychological interventions on subjective and objective outcomes. The
result has shown that the addition of psychological interventions to
exercise-based cardiac rehabilitation showed a trend to reduce depressive
symptoms (standardized mean difference –0.13, 95% confidence interval (CI)
–0.30 to 0.05) and cardiac morbidity (risk ratio 0.74, 95% CI: 0.51 to 1.07) [26].
The cardiac morbidity considered were any non-fatal cardiovascular events
including percutaneous coronary intervention, coronary artery bypass grafting,
stroke or peripheral revascularization, and emergency visits. Similarly,
Dusseldorp et al. [27] analyzed 37 studies to evaluate the effects of
psychoeducational in CAD patients. The corresponding reduction in cardiac
mortality and recurrence of myocardial infarction noted in patients who attended
the programs were 34% and 29% (p
Milani et al. [28] has concluded that exercise training helps in
reducing psychosocial stress and associated mortality in patients with coronary
artery disease. The study has noted 4-fold increased mortality in patients with
high psychosocial stress as opposed to those with low psychosocial stress (22%
vs 5%; p = 0.003). Exercise training contributed to the decrease in the
prevalence of psychosocial stress from 10% to 4% (p
On contrary, a 2003 study by Sundin et al. [17] has reported no significant difference in coronary risk reduction upon comparing residential/outpatient multifactorial cardiac rehabilitation, stress management, and standard coronary rehabilitation. The randomized study included 132 male patients who had undergone percutaneous transluminal coronary angiography, coronary artery bypass graft, or acute myocardial infarction. However internal locus of control, self-reported healthy diet habits and exercise frequency were significantly higher in patients who received behavioral rehabilitation [17]. Similarly, Plüss et al. [30] has concluded that expanded cardiac rehabilitation does not confer any significant benefit on biochemical risk markers or in exercise performance among patients treated for an acute myocardial infarction or a coronary artery bypass graft operation.
The present meta-analysis has several limitations. Since the meta-analysis included only a limited number of studies, estimating between-study heterogeneity was challenging. Since there is no universally accepted single measure or gold standard for measuring stress, studies differ in the measures adopted for the evaluation of stress. Hence the present study could not consider daily stress behavior score, HAF-17, and QoL for meta-analysis due to an insufficient number of studies. In addition, the literature review shows that there are very limited studies evaluating the incidence of angina, hospitalization and other adverse cardiac outcomes in patients who received stress management training as a part of cardiac rehabilitation. Hence the present meta-analysis could not consider these variables. Since the study was mainly focused on cognitive behavioral therapies, it did not consider exercise-based articles as a systematic review has been published recently [31]. In addition, there was no study evaluated the effect of stress management program in subjects with myocardial infraction fulfilling the present inclusion and exclusion criteria. Another major limitation is not investigating the extracted data independently by the reviewers.
The present study holds significant relevance, as it is one of its kind evaluating the role of stress management among CAD and MI patients through meta-analysis. The study highlighting the benefits of stress management training in cardiac rehabilitation may assist in developing guidelines advocating the incorporation of stress management training in comprehensive cardiac rehabilitation. By moving forward, it is necessary to standardize the measures that are crucial for stress management evaluation through evidence-based trials and to develop consensus on the use of such measures in routine medical care.
The present systematic review and meta-analysis largely concurs with those of earlier clinical trial studies and suggesting the benefits of stress management in patients undergoing cardiac rehabilitation. Newer research areas should focus on standardization of stress management instruments, customization of these tools based on the patient’s disease profile, and developing evidence-based guidelines for adoption of stress management program combined with cardiac rehabilitation.
Conceptualization and Project administration—YS and JL; Data curation, Formal analysis and Methodology and using software—YS; Supervision and Validation—JL; Writing the original draft—YS and JL. All authors have read and approved the manuscript.
Not applicable.
We would like to express our gratitude to all those who helped us during the writing of this manuscript. Thanks to all the peer reviewers for their opinions and suggestions.
This research received no external funding.
The authors declare no conflict of interest.
The datasets generated and analyzed during the present study are available from the corresponding author upon request.
