Background: Off-pump coronary artery bypass grafting (OPCAB) is an
alternative to on-pump coronary artery bypass grafting (CABG) with
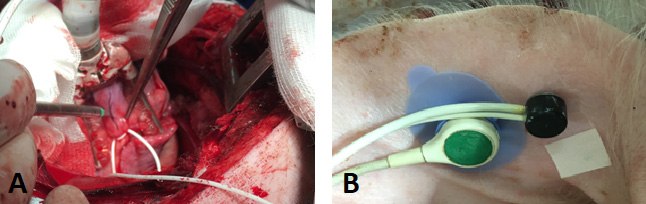
cardiopulmonary bypass (CPB). During OPCAB, the temporary use of an intracoronary
shunt and inotropic medication or catecholamines should keep the central
hemodynamics constant. Nevertheless, the need for conversion to on-pump CABG
often occurs unexpectedly, most likely due to circulation instability.
Circulation instability can appear first in peripheral body parts; therefore,
peripheral microcirculation might serve as a predictor for the upcoming
conversion to on-pump CABG. We investigated the impact of coronary artery
ligation and shunt insertion during OPCAB on cutaneous microcirculation (cLDP)
with Laser Doppler Perfusion Technology and transcutaneous oxygen partial
pressure (tcpO). Methods: In a pig model of OPCAB, peripheral
circulation was evaluated after cLDP (N = 17) and tcpO (N = 6) monitoring.
Systolic, diastolic, and mean arterial pressure were also observed to prove the
independence of perfusion measurement results from hemodynamic parameters.
Results: Ligation time during cLDP and tcpO monitoring were 101
49 s and 83 33 s, respectively. Shunt time was 11 3 min
during cLDP and 13 2 min during tcpO measurement. Ligation of the
left anterior descending coronary artery (LAD) reduced cLDP significantly to 88
14% (p = 0.007) and tcpO to 71 25% (p =
0.038). Inserting a temporary shunt into the LAD significantly improved cLDP
(p = 0.006) and tcpO (p = 0.015) compared to ligation.
cLDP was restored to 99%, and tcpO was restored to 91% of the baseline
level before ligation. All hemodynamic parameters remained stable and did not
change significantly during OPCAB. Conclusions: Although hemodynamic
parameters stayed constant, peripheral microcirculation was influenced markedly
during OPCAB. Inserting a temporary shut into the LAD leads to a complete
normalization of peripheral microcirculation, regarding evaluation by cLDP and
tcpO.