Background: Atrial fibrillation (AF) is an indicator of frailty in old
patients. This study aimed to investigate the effect of frailty on the use of
oral anticoagulants (OAC) and clinical outcomes in a nationwide cohort of
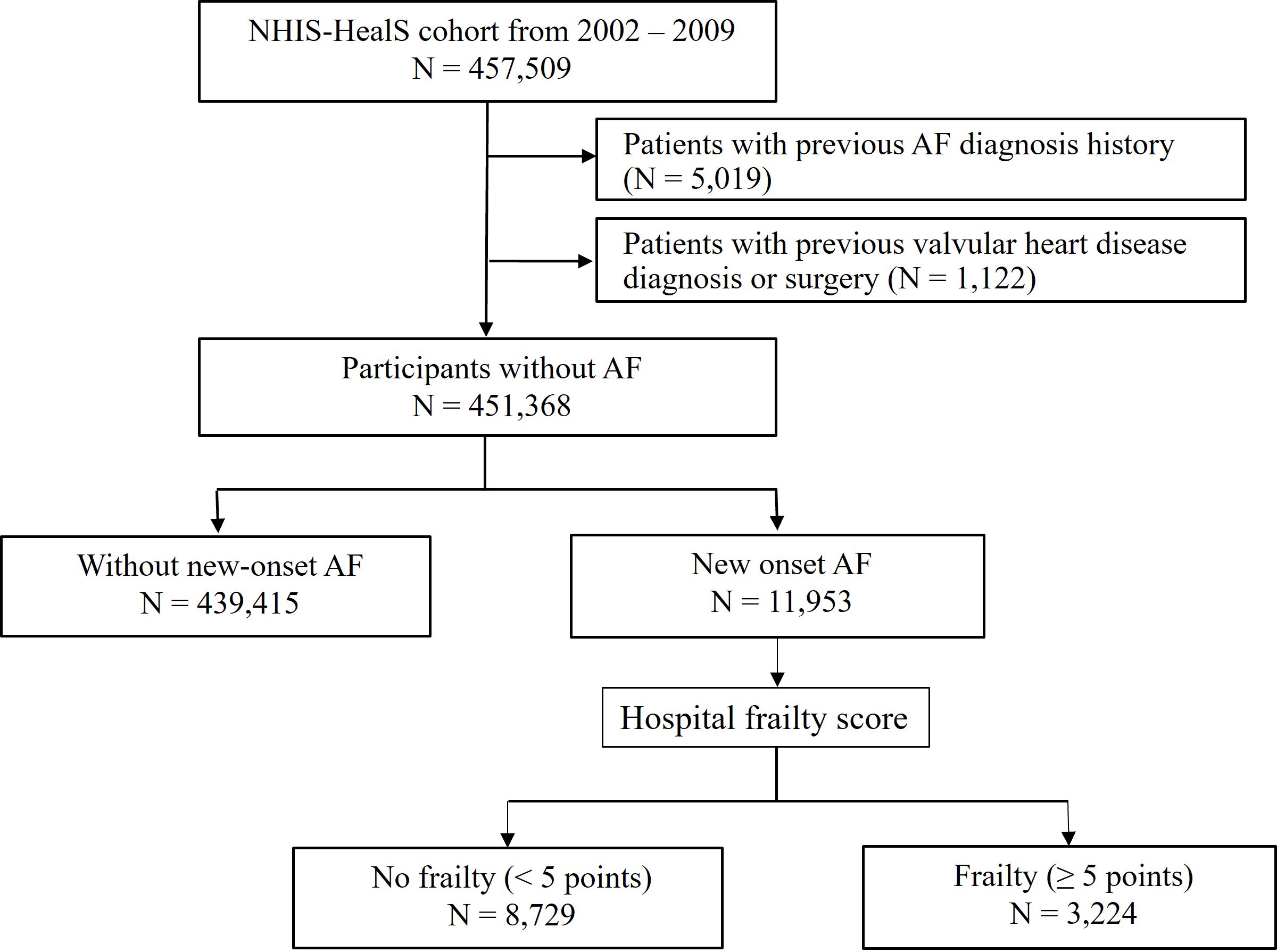
patients with new-onset AF. Methods: This study included 451,368
participants without AF from the Korea National Health Insurance Service-Health
Screening cohort between 2002 and 2009. The Hospital Frailty Risk Score was
retrospectively calculated for each patient using all available International
Classification of Disease 10th revision diagnostic codes. According to the
aggregate score, patients were divided into two groups: the participants without
frailty (5 points) and the participants with frailty (5 points). The
primary outcome was death from any cause, and the secondary outcomes were
cardiovascular death, ischemic stroke, major bleeding, and heart failure
admission. Results: With up to 7.2 1.5 years of follow-up,
11,953 participants (median age, 67 [interquartile range, 59.5–74.5] years; 7200
[60.2%] males) developed new-onset AF. Among the patients with AF, 3224 (26.9%)
had frailty. Frailty was significantly associated with old age, female sex,
polypharmacy, and other comorbidities. In patients with AF, frailty was
negatively associated with OAC prescription after new-onset AF (p
0.001). Compared to patients without frailty, patients with frailty had a
significantly higher incidence and risk of all-cause death (hazard ratio [HR]
2.88, 95% confidence interval [CI] 2.65–3.14), cardiovascular death (HR 2.42,
95% CI 2.10–2.80), ischemic stroke (HR 2.25, 95% CI 2.02–2.51), major
bleeding (HR 2.44, 95% CI 2.17–2.73), and heart failure admission (HR 1.29,
95% CI 1.09–1.52). In subgroup analysis, when compared to the non-OAC group,
the risks associated with frailty were significantly lower in the OAC group for
all-cause death, cardiovascular death, ischemic stroke, and heart failure
admission. Conclusions: Frailty was negatively associated with the use
of OAC and was a predictor of poor prognosis owing to the association of frailty
with death, thromboembolic events, bleeding, and heart failure admission.
However, OAC use was associated with lower risks related to frailty for all-cause
death and major adverse cardiovascular events in patients with AF.