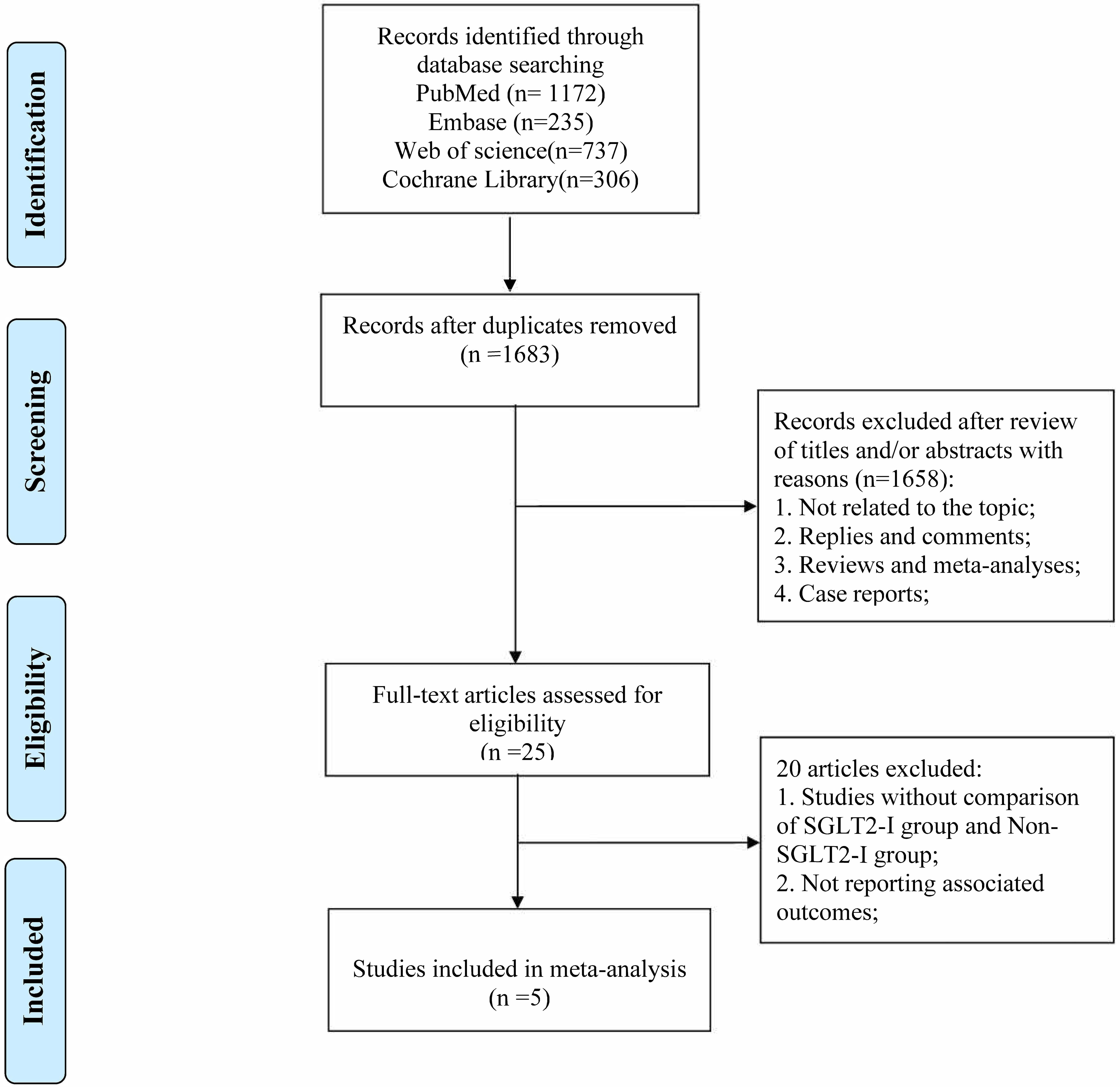
Background: The present meta-analysis aimed to examine the effects of sodium-glucose cotransporter 2 (SGLT2) inhibitors on the prognosis of diabetes patients who experienced acute myocardial infarction (AMI). This investigation encompassed an array of clinical endpoints, comprising cardiovascular death, myocardial reinfarction, all-cause mortality, major adverse cardiovascular events (MACEs), and rehospitalization. Methods: The study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The PubMed, Cochrane Library, Embase, and Web of Science databases were searched up to October 2023. Studies reporting clinical outcomes in diabetic patients who experienced AMI and were treated with SGLT2 inhibitors (SGLT2-I) were included. Two researchers independently selected the studies and assessed the risk of bias in the included studies using the Cochrane risk of bias tool for Risk for Bias In Non-randomized Studies-of Interventions (ROBINS-I). Results: A total of 2450 publications were initially retrieved; ultimately, five studies involving 5398 patients were included in the meta-analysis. The analysis revealed that SGLT2-I were associated with significantly lower risks of cardiovascular death (odds ratio (OR), 0.34; 95% CI, 0.14–0.82) and all-cause mortality (OR, 0.54; 95% CI, 0.38–0.76). However, SGLT2-I did not lead to a significant decrease in the rate of myocardial reinfarction (OR, 0.91; 95% CI, 0.65–1.29). SGLT2-I did lead to a significant reduction in MACEs (OR, 0.59; 95% CI, 0.35–1.0), but there was significant heterogeneity among the included studies. SGLT2-I also led to a significant reduction in rehospitalizations (OR, 0.45; 95% CI, 0.26–0.76). There was significant heterogeneity in the analysis of rehospitalization, but the effect remained significant when we excluded the main sources of heterogeneity (OR, 0.35; 95% CI, 0.24–0.52). Conclusions: The pooled analyses revealed that SGLT2-I were associated with reductions in all-cause mortality, cardiovascular death, and rehospitalization. In the future, prospective studies with larger sample sizes are needed to confirm and refine these findings.