Background: The main objective of this study was to determine whether
myocardial strain and myocardial work are altered in hypertension and whether
the strain is independent of hypertension-induced left ventricular hypertrophy.
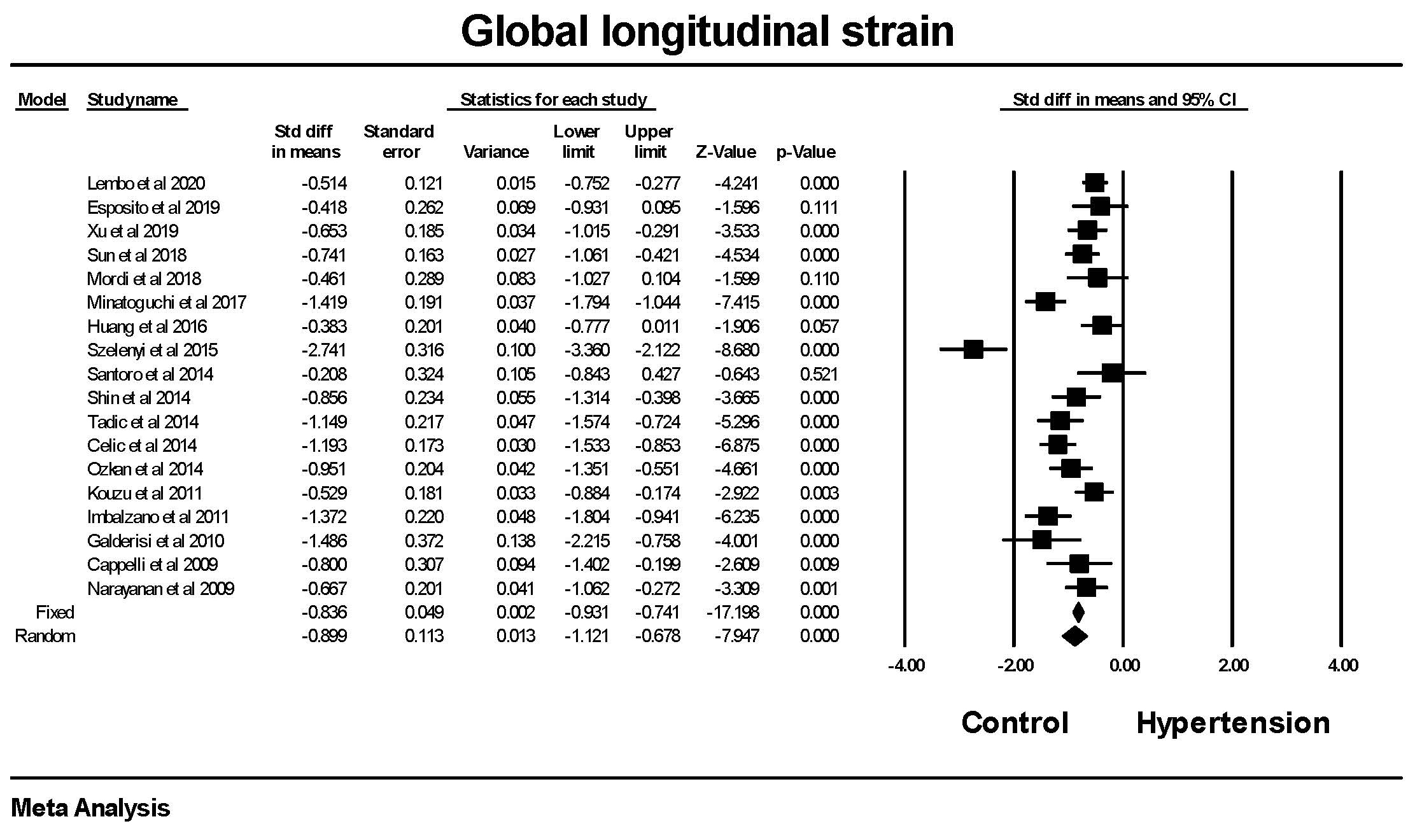
Methods: Two systematic literature searches were conducted using Medline
and EMBASE through to June 30, 2022. In the first, search terms left
ventricular strain or speckle tracking AND hypertension and left
ventricular hypertrophy were used in conjunction with Boolean operators to
identify articles reporting left ventricular strain in patients with
hypertension. In the second, the terms Global cardiac or myocardial work AND
hypertension were used to identify articles. Publication bias was assessed by
examination of funnel plots and calculation of the Failsafe N and Duval and
Tweedie’s Trim and fill. The results were presented as Forrest plots.
Results: Global longitudinal strain (GLS) was significantly lower in
patients with hypertension compared to those without hypertension with a mean
difference of 2.0