Background: Elevated levels of troponin-I (TnI) are common in
out-of-hospital cardiac arrest (OHCA) patients. However, studies evaluating the
prognostic value of TnI clearance in OHCA patients are lacking. We aimed to
examine how TnI clearance (TnI-C) differed according to the neurological outcome
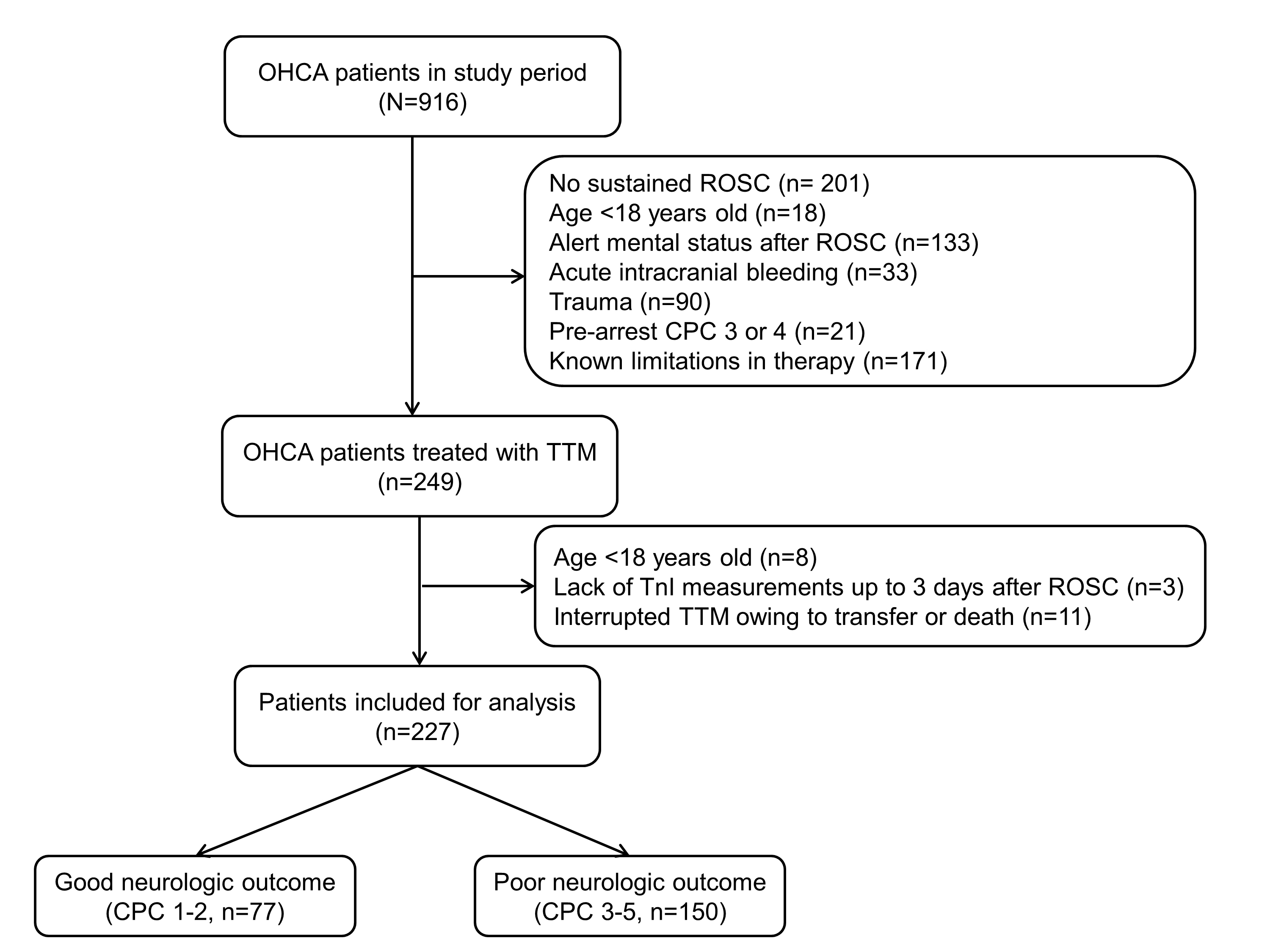
group and mortality group at 6 months. Methods: This retrospective
observational study involved adults (18 years) who were treated for an
OHCA between January 2019 and December 2022. The TnI-Cs were calculated for days
1 to 2 (TnI-C1st) and 2 to 3 (TnI-C2nd) after the return of spontaneous
circulation (ROSC). The primary outcome was a poor neurological outcome at 6
months, defined by cerebral performance categories 3, 4, and 5. The secondary
outcome was 6-month mortality. Results: A total of 227 patients were
included. A poor neurological outcome and mortality at 6-months were reported in
150 (66.1%) and 118 (52.0%) patients, respectively. The TnI-C1st was
significantly lower in patients with a poor outcome compared with good outcome
patients (neurological outcome at 6 months, 54.4% vs. 42.3%; 6-month mortality,
52.1% vs. 42.7%, respectively). In the multivariable analyses, a TnI-C1st 50% was associated with a poor neurological outcome (odds ratio [OR] 2.078,
95% confidence interval [CI] 1.080–3.995, p = 0.028) and mortality (OR
2.131, 95% CI 1.114–4.078, p = 0.022) at 6 months.
Conclusions: After ROSC, TnI-C1st 50% was associated with a
poor neurological outcome and mortality at 6 months in OHCA patients.