†These authors contributed equally.
Background: Hypertensive patients with obstructive sleep apnea (OSA)
are at a high risk of cardiovascular disease (CVD), but assessments of CVD risk
in this population are frequently constrained by the presence of comorbid medical
conditions. The noninvasive and convenient hepatic steatosis index (HSI) can not
only predict the degree of fatty liver degeneration but also correlates well with
the severity of numerous diseases. However, the relationship between the HSI and
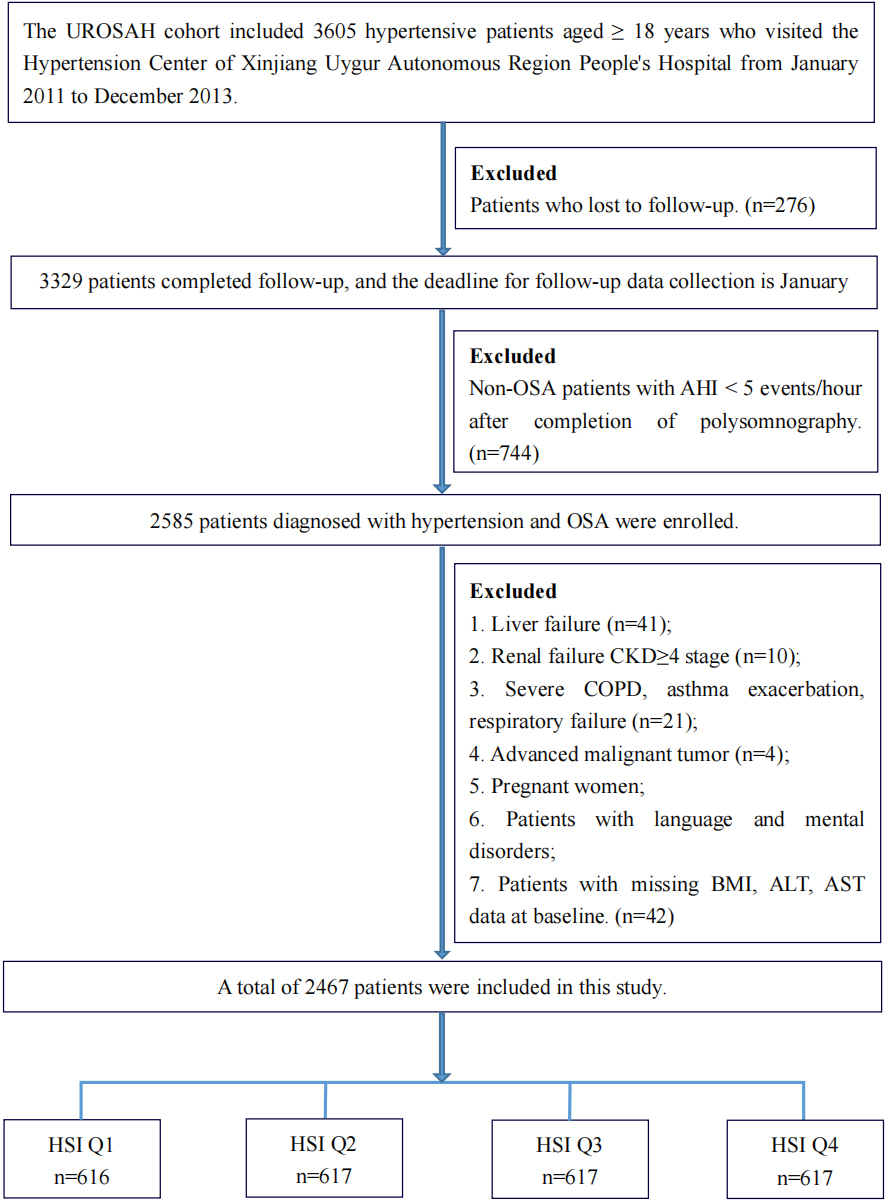
CVD in hypertensive patients with OSA remains unclear. Methods: This
retrospective cohort study included patients aged